Ever felt your stomach tie itself in knots when stress hits? For millions of Americans, that unsettling sensation isn’t just a fleeting feeling; it’s a constant, debilitating reality known as Irritable Bowel Syndrome, or IBS. This isn’t your average stomachache; it’s a chronic condition marked by abdominal pain, bloating, gas, and unpredictable swings between diarrhea and constipation. While IBS affects roughly one in ten people globally, its exact causes have remained largely mysterious, leading to treatments that mostly just manage symptoms, like putting a bandage on a deeper wound. But what if the key to unlocking relief for IBS sufferers isn’t found in the gut itself, but in the intricate command center of our very being—the brain? Groundbreaking new research from the Tokyo University of Science suggests just that, potentially flipping our understanding of IBS on its head and offering a fresh approach to tackling this pervasive condition.
The Brain-Gut Connection: A Deeper Look at IBS
For years, doctors have noticed a strong link between psychological stress and IBS. We all know that feeling of “nervous butterflies” before a big event, which clearly shows how closely our brain and gut are connected. This connection, often called the “gut-brain axis,” involves complex signals traveling between our brain and spinal cord (the central nervous system) and the “brain of the gut” (the enteric nervous system). When we’re stressed, our brain releases chemicals that can directly affect how our gut works, leading to classic IBS symptoms. Professor Akiyoshi Saitoh’s team at Tokyo University of Science has spent the last decade digging into this detailed relationship, driven by the idea that if stress plays such a big role, perhaps the solution lies in addressing how the brain handles that stress.
To study this, Professor Saitoh’s group first needed a reliable way to observe stress-induced IBS in a controlled setting. They built on their earlier work, developing a unique mouse model in 2022. These mice were exposed to what’s called “chronic vicarious social defeat stress” (cVSDS). In plain language, these mice repeatedly watched another mouse being aggressively defeated by a dominant mouse. This method mimicked the kind of ongoing, emotional strain that often worsens IBS in humans, without the mice themselves being physically harmed. The results were clear: after this stressful experience, the cVSDS mice developed symptoms strikingly similar to diarrhea-predominant IBS (IBS-D), including overly active intestines and increased sensitivity to abdominal pain, even without any physical damage to their digestive systems. This confirmed the cVSDS model as a powerful tool for understanding the brain’s role in IBS.
Opioid Receptors in the Brain: A New Path to Relief
With their animal model established, the researchers turned their attention to a specific target in the brain: opioid delta-receptors (DOPs). It’s important to understand that these receptors are naturally present in the brain and are crucial for managing pain, mood, and stress responses. They are different from the opioid receptors targeted by common pain medications, and the drugs studied here, called DOP agonists, are designed to activate these specific receptors with minimal side effects. The central question was whether activating these DOPs in the brain could ease the IBS-like symptoms in their stressed mice.
To investigate this, the team performed several careful experiments. One key test was the “charcoal meal test,” where mice were given a meal mixed with charcoal, and the researchers then measured how quickly the charcoal moved through the small intestine. An overly active intestine, typical of IBS-D, would show faster transit. They also used a “capsaicin-induced hyperalgesia test,” where a mild irritant (like the compound that makes chili peppers hot) was administered to measure abdominal pain sensitivity by observing the mice’s pain-related behaviors.
When the researchers administered KNT-127, a DOP agonist, to the cVSDS mice, the drug made a noticeable difference. It was given in two ways: as an injection into the body and directly into the brain. Both methods helped normalize the mice’s overly active intestines and reduced signs of abdominal pain. To further confirm that the drug was working in the brain, they used another DOP agonist, SNC80, which showed similar improvements when given directly into the brain. Crucially, when they blocked the DOPs in the brain using a specific inhibitor, the positive effects of KNT-127 disappeared. This strongly indicated that the drug was acting on the brain, not directly on the gut, to provide relief.
Targeting the Insular Cortex: A Key Brain Region
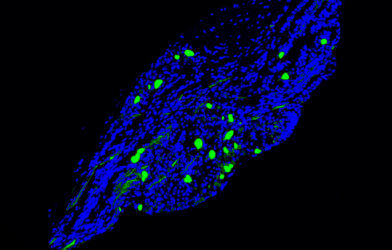
The brain is incredibly complex, so identifying the exact area where these DOP agonists were having their effect was the next critical step. The researchers focused on the insular cortex, a fascinating part of the brain linked to processing emotions, pain, and even regulating our internal organs through the autonomic nervous system—the system that controls involuntary bodily functions like digestion and heart rate. Past studies had shown that DOPs are highly concentrated in this specific brain region.
To test the insular cortex’s role, the team directly infused KNT-127 into this area in the cVSDS mice. The results were striking: this local infusion, even in very small amounts, normalized the increased intestinal activity in a way that depended on the dose. This was a significant finding, indicating that the insular cortex is a key player in how these drugs improve IBS symptoms. To understand the underlying mechanism, the researchers used a technique called in vivo brain microdialysis, which allowed them to measure levels of brain chemicals like glutamate. They found that in chronically stressed mice, re-exposure to stress significantly increased glutamate levels in the insular cortex. Importantly, administering KNT-127 suppressed this surge in glutamate. This suggests that in stressed individuals, the insular cortex might become overactive due to too much glutamate, contributing to IBS symptoms, and that DOP agonists work by calming this overactivity.
Hope for Millions: A New Era for IBS Treatment
These findings propose a compelling new direction for IBS treatment. Current therapies largely manage symptoms, often with limited success and patient satisfaction. The idea of a drug that not only addresses painful gut symptoms but also helps regulate the underlying stress and emotional distress common with IBS is a game-changer. As Professor Saitoh notes, “Our findings demonstrated that DOP agonists acted directly on the central nervous system to improve diarrhea-predominant IBS symptoms in mice, and suggest that the mechanism of action involves the regulation of glutamate neurotransmission in the insular cortex.”
This research paves the way for developing medications that offer a “radical treatment” for IBS, working through a mechanism fundamentally different from existing options. Instead of simply slowing down an overactive bowel or easing pain with general remedies, these new drugs could rebalance brain chemistry for more comprehensive relief. While this research was conducted in mice and human trials are needed, the discovery that targeting the brain’s opioid delta-receptors, particularly in the insular cortex, can alleviate stress-induced IBS-like symptoms is a significant leap forward. The path to effective, root-cause treatments for IBS appears clearer than ever, offering a beacon of hope for millions.
Paper Summary
Methodology
The study used male C57BL/6J mice exposed to “chronic vicarious social defeat stress” (cVSDS) to induce IBS-D-like symptoms. Researchers evaluated intestinal motility via the charcoal meal test and abdominal pain sensitivity using the capsaicin-induced hyperalgesia test. Brain microdialysis measured glutamate levels in the insular cortex. The selective opioid delta-receptor (DOP) agonist KNT-127 was administered through various routes, with blinding of investigators for objectivity.
Results
KNT-127 significantly regulated intestinal movement and relieved abdominal pain in cVSDS mice when administered systemically or directly into the brain. An inhibitor blocked these effects, confirming the drug’s action in the central nervous system. Direct infusion of KNT-127 into the insular cortex also improved intestinal hypermotility. The drug suppressed stress-induced increases in glutamate levels in the insular cortex, suggesting it calms overactivity in this brain region.
Limitations
The study focused solely on IBS-D-like symptoms due to the lack of an IBS-C animal model. Assessing precise pain relief from brain-cannula implantation was challenging. The research did not pinpoint specific subregions within the insular cortex or definitively rule out other neurotransmitters or neural circuits.
Funding and Disclosures
This work was supported by the Japan Agency for Medical Research and Development (AMED, grant number JP24gm1510008). The authors declared no conflicts of interest.
Publication Information
Yoshioka, T., Kimiki, S., Yamazaki, M., Hamano, T., Ou, M., Ode, Y., Ehara, R., Kajino, K., Kasai, S., Yoshizawa, K., Saitoh, T., Yamada, D., Nagase, H., & Saitoh, A. (2025). Agonists of the opioid δ-receptor improve irritable bowel syndrome-like symptoms via the central nervous system. British Journal of Pharmacology, 182(7), 1599–1609. https://doi.org/10.1111/bph.17428