For American parents, the quest for a healthy baby starts long before birth. We diligently track our cycles, take prenatal vitamins, and avoid certain foods, all in the hope of giving our children the best possible start. But what if one of the most powerful tools for a baby’s development isn’t a new supplement or a diet plan, but is already living inside the mother’s gut?
This isn’t a new health craze—it’s a powerful takeaway from a groundbreaking new study. Scientists now believe a common “good bacteria” called Bifidobacterium breve plays a crucial role in shaping a healthy fetal brain. The research suggests that a pregnant mother’s gut health may be as vital for a baby’s development as diet and prenatal care. It’s a concept that opens the door to a new way of thinking about how we support a healthy pregnancy.
A Microscopic Bridge to the Brain
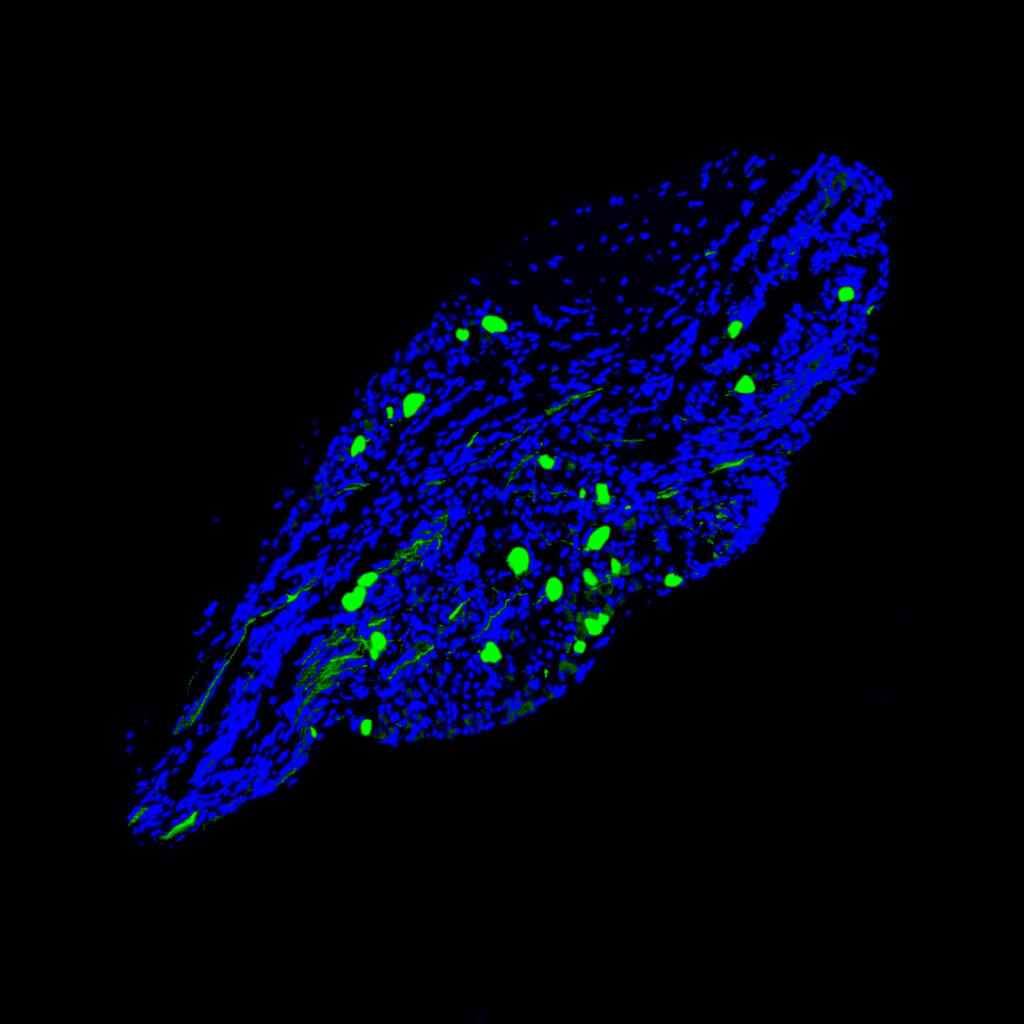
To understand how bacteria in the gut can affect a baby’s brain, we need to think about the incredible connection between a mother and her fetus. The study found that when a pregnant mouse’s gut was rich in Bifidobacterium breve, these microbes seemed to act as a bridge, boosting the transport of key nutrients from the mother to the baby’s developing brain. This is crucial because a fetal brain is a ravenous consumer of energy, and its growth depends entirely on a steady supply of nutrients.
The research also found that the bacteria were linked to elevated levels of critical proteins and pathways that are essentially the blueprints for healthy brain development. For example, they saw an increase in a key mitochondrial complex. Mitochondria are the powerhouses of our cells, and this finding indicates that the bacteria might be giving the fetal brain a supercharged environment for growth and development.
How the Study Worked
To isolate these effects, researchers used a special group of pregnant mice known as “germ-free” mice, meaning they had no bacteria in their guts. This allowed the scientists to precisely control the environment and see what happened when they introduced just one type of bacteria. One group of mice was given Bifidobacterium breve orally during their pregnancy, while the control group remained germ-free. The scientists then carefully analyzed the fetal brains to compare them.
The study, which was published in the journal Molecular Metabolism, found that ten specific metabolites, including key amino acids and citrate, were significantly reduced in the fetal brains of the treated group. While this might sound bad, the researchers interpret it as a positive sign, suggesting that these nutrients were being consumed at a faster rate due to the increased growth and metabolic activity in the brain. It’s like a construction site with a high-speed conveyor belt: the raw materials are being used so quickly that the stock of them remains low.
What This Means for Parents
While this study was conducted on mice, the researchers believe that the effects are likely similar in humans. The findings could pave the way for a new era of proactive prenatal care where a woman’s gut health is recognized as a vital pillar of a baby’s future. It provides a potential roadmap for a drug-free way to support fetal development.
This research highlights that the smallest things—in this case, microscopic bacteria—can have the most profound impact on our health. It’s a powerful reminder that our bodies, and the lives they create, are complex ecosystems, and sometimes, the best way to nurture them is to tend to the garden within.
Paper Summary
Methodology
The study used two groups of pregnant, germ-free mice (meaning they had no bacteria in their guts). One group was given the bacterium Bifidobacterium breve orally during pregnancy, while the other group served as the untreated control. Fetal brains were then analyzed to compare their metabolic profiles, including metabolites, gene expression, and cellular pathways. The study analyzed 9 fetuses per group, from a total of 5 pregnant dams in the untreated group and 6 in the treated group.
Results
Maternal colonization with B. breve led to significant changes in the fetal brain. Ten specific metabolites, including several amino acids and citrate, were reduced in the brains of the treated fetuses. The study also found an increased abundance of nutrient transporters for glucose and branched-chain amino acids. Additionally, the bacterium was associated with elevated levels of proteins and pathways related to cell growth and metabolism, such as the PI3K-AKT and Wnt-β-catenin signaling pathways, and stabilization of the HIF-2α protein.
Limitations
The study was conducted on germ-free mice, which allowed for precise control but is not representative of a natural human pregnancy. The authors state that while the effects are likely to be similar in humans, more research is needed to understand how the findings translate to people. Future studies should include additional control groups and perform structural analyses to determine if the bacterial treatment leads to visible changes in the brain’s physical structure, such as cell division or axon development.
Funding and Disclosures
The provided document does not contain an explicit “Funding” section.
Publication Information
The article, “Maternal gut Bifidobacterium breve modifies fetal brain metabolism in germ-free mice,” was published in the journal Molecular Metabolism. The authors include Jorge Lopez-Tello, Raymond Kiu, Zoe Schofield, Cindy X.W. Zhang, Douwe van Sinderen, Gwénaëlle Le Gall, Lindsay J. Hall, and Amanda N. Sferruzzi-Perri. The paper was received on June 3, 2024, accepted on August 6, 2024, and made available online on August 8, 2024.