
Microbiome

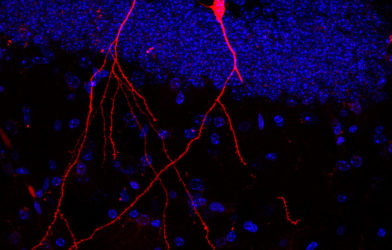
Microscopic ‘vehicles’ enable gut bacteria to stimulate the brain and other organsJanuary 14, 2022

Severe COVID-19 linked to poor gut healthJanuary 14, 2022

Gut health is compromised during chemotherapy, study findsJanuary 13, 2022

How 35-year-old stool samples shed light on the gut’s role in HIV/AIDSJanuary 13, 2022

Triclosan, an antibacterial in toothpaste and toys, harms gut healthJanuary 13, 2022

Plant-based diets are great for your heart — and your gut, tooJanuary 12, 2022
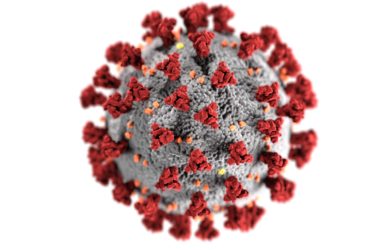
Harvard’s ‘intestine chip’ may help solve gut issues related to COVIDJanuary 12, 2022

Concerning rise in colorectal cancer among young people points to gut bacteriaJanuary 12, 2022
