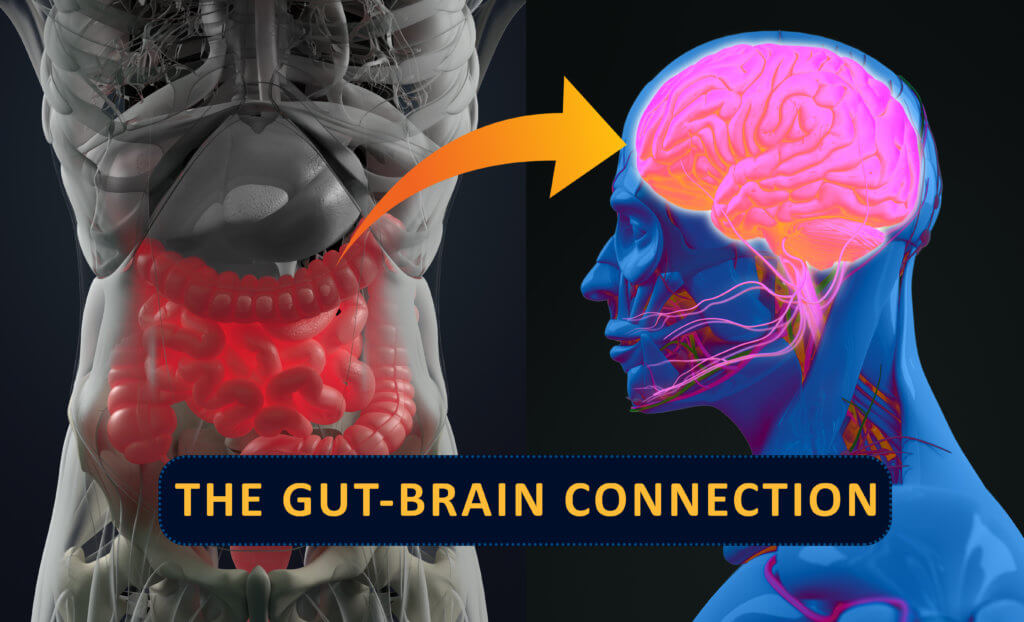
If you’ve ever felt a wave of anxiety wash over you before a big presentation, or if stress has ever given you a knot in your stomach, you’ve experienced the gut-brain axis in action. This isn’t just a quirky figure of speech; it’s a constant, two-way biological highway where signals, hormones, and billions of tiny organisms in your digestive tract directly influence your mood, your mental health, and the health of your nervous system.
For millions of Americans living with Parkinson’s disease (PD), the symptoms—tremors, slowed movement, stiffness, and loss of balance—are a daily, progressive struggle. PD is a neurodegenerative disorder, meaning it slowly breaks down the essential nerve cells in the brain that control movement. The world of medicine has been searching for a way to slow or stop the disease, and a groundbreaking new international study has revealed a startling possibility: The key to a major breakthrough might lie in a simple, common vitamin. Researchers have found a crucial link between the health of the bacteria living in your intestines and the progression of Parkinson’s. Their work points to a deficiency of two common B vitamins—riboflavin (B2) and biotin (B7)—in the gut as a potential major contributor to the disease.
Tracing Parkinson’s to the Gut’s Ecosystem
The research, led by Dr. Hiroshi Nishiwaki from Japan’s Nagoya University Graduate School of Medicine, didn’t rely on a single, small test group. The team performed what’s known as a meta-analysis, a powerful technique that allows scientists to combine and analyze data from multiple existing studies, treating them as one massive, global dataset. The researchers added their own data, which included 94 Parkinson’s patients and 73 healthy individuals from Japan, to five other previously published studies from the United States, Germany, China, and Taiwan. Combining information from diverse populations helped the team ensure the patterns they found weren’t just specific to one diet or region.
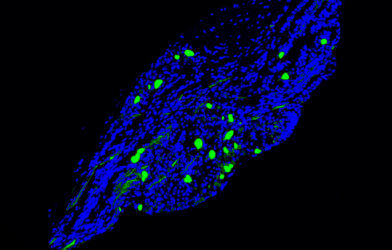
To understand the microbial ecosystem inside the gut, the scientists used a sophisticated lab technique called shotgun sequencing. This method is a complete reading of the full genetic blueprint of every microbe in a given stool sample. By mapping all the genes present, the researchers could tell exactly what the bacteria were capable of doing, not just what species they were. The data points to a major finding: Parkinson’s patients had a significant decrease in the genes responsible for the biosynthesis—the natural creation—of riboflavin and biotin. Further analysis revealed that specific bacteria species known to produce beneficial chemicals, namely Roseburia intestinalis and Faecalibacterium prausnitzii, were also decreased.
The Gut’s Protective Shield is Failing
Once the genetic data showed a deficiency in B vitamin-making genes, the research team looked at the chemical aftermath. They measured the levels of specific protective molecules in the fecal samples, focusing on short-chain fatty acids (SCFAs) and polyamines. These beneficial molecules, produced by healthy gut bacteria, are essential for maintaining the intestinal barrier.
The intestinal barrier functions like a protective shield or a tightly woven fence along the inner wall of your gut. Its critical job is to allow beneficial nutrients to pass into the bloodstream while keeping out harmful bacteria, toxins, and unwanted substances. The data showed that levels of both SCFAs and polyamines were significantly lower in the Parkinson’s patients. This finding clearly indicates a connection: fewer vitamin-making genes resulted in lower levels of protective molecules.
When the levels of these protective molecules drop, the intestinal barrier thins and becomes more permeable—it develops holes. This condition is what allows toxic substances to enter the body. Dr. Nishiwaki explained the mechanical result: “This higher permeability exposes nerves to toxins, contributing to abnormal aggregation of alpha-synuclein, activating the immune cells in the brain, and leading to long-term inflammation.”. Alpha-synuclein is the protein that misfolds and clumps into sticky deposits, damaging the nerve cells critical for movement and driving the symptoms of Parkinson’s disease.
A Simple Solution for a Complex Disease
The findings offer a surprisingly simple and accessible approach to treatment. Instead of relying on the development of complex, expensive new medications, this avenue of research suggests the possibility of using readily available oral dietary supplements. Riboflavin and biotin are affordable, common B vitamins.
Dr. Nishiwaki noted that supplementation therapy targeting riboflavin and biotin “holds promise as a potential therapeutic avenue for alleviating PD symptoms and slowing disease progression.”. The possibility here is a revolutionary change in how we manage the disease. In the future, a doctor could analyze a patient’s gut profile—or conduct fecal metabolite analysis—to identify specific deficiencies and then administer supplements to address the problem directly.
This study provides a critical step forward in understanding Parkinson’s disease, powerfully highlighting the intricate link between our digestive health and our neurological well-being. By finding a tangible, accessible target like a simple vitamin deficiency, researchers have opened a new path that moves beyond simply managing symptoms and aims to address a potential root cause of the disease. This discovery underscores that the path to brain health may begin with a healthier gut.
Paper Summary
Methodology
The study was a meta-analysis combining a new dataset of 94 Parkinson’s disease (PD) patients and 73 controls from Japan with five existing international datasets. Researchers used shotgun sequencing to map the genes of the gut microbiota and advanced laboratory assays (GC-MS and LC-MS/MS) to quantify short-chain fatty acids (SCFAs) and polyamines in fecal samples.
Results
The gut microbial diversity was increased in PD patients across the combined datasets. The key finding was a significant decrease in bacterial genes responsible for the biosynthesis of riboflavin (B2) and biotin (B7), alongside a corresponding decrease in the levels of beneficial molecules like SCFAs and polyamines.
Limitations
Key limitations included the use of data from different countries (introducing potential dietary variables), the cross-sectional nature of the study (meaning it cannot confirm cause vs. consequence), and the inability to fully adjust for the potential effects of all patient medications.
Funding and Disclosures
The research was supported by grants from the Japan Society for the Promotion of Science (JSPS) KAKENHI, the Daiichi Sankyo Foundation of Life Science, the Naito Foundation, the Japan Agency for Medical Research and Development (AMED), and the Parkinson’s Foundation. The authors stated they had no competing interests to disclose.
Publication Information
This research paper, titled “Meta-analysis of shotgun sequencing of gut microbiota in Parkinson’s disease,” was published in the journal npj Parkinson’s Disease in 2024. The paper’s DOI is https://doi.org/10.1038/s41531-024-00724-z.