More than half of the U.S. adult population take prescription drugs – making America the pill nation of the world. The majority of these adults are 80 or older and suffer from severe conditions such as diabetes and cardiovascular disorders, according to Georgetown University’s Health Policy Institute. While these medicines may help alleviate certain symptoms, a recent study reveals the damaging effects they have on the beneficial microbes in the gut.
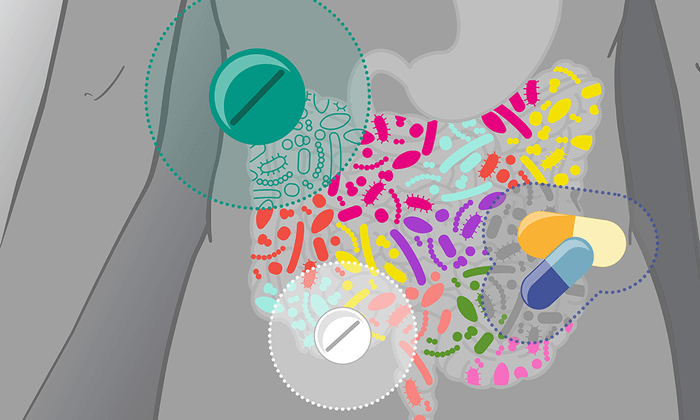
Billions of bacteria populate the gut, working together to fight off harmful microbes and carry out metabolic processes like digestion and nutrient absorption. In essence, the microflora of the gut is necessary for the body to function properly. When the body experiences sickness, or in many cases pharmaceutical drugs, the microbiome is altered which often has a negative outcome.
For example, antibiotics, prescribed to combat harmful bacteria, do so by wiping out all of the bacteria within the body. They are not capable of discriminating between beneficial and harmful microbes. Because of this unbalanced microflora, the body has no healthy bacteria to carry out critical functions, and, sometimes harmful bacteria in the body overpopulates.
In a recent comprehensive study, scientists from EMBL Heidelberg’s Bork group analyzed the effects of drugs such as antibiotics and cardiovascular medications on the body’s microbiome. “We analyzed the effects of 28 different drugs and several drug combinations. Many drugs negatively impact the composition and state of the gut bacteria, but others, including aspirin, can have a positive influence on the gut microbiome. We found that drugs can have a more pronounced effect on the host microbiome than disease, diet, and smoking combined,” says Peer Bork, Director of Scientific Activities at EMBL Heidelberg.
Previous studies show the harmful effects of prescriptions on healthy gut bacteria, however, this research reveals a possible cumulation of the detrimental impact of drugs over time. “We found that the gut microbiome of patients taking multiple courses of antibiotics over five years became less healthy. That included signs indicating antimicrobial resistance,” says Sofia Forslund, co-first author of the study, and a former postdoctoral fellow in the Bork group. She is also currently the group leader at the Max Delbrück Center for Molecular Medicine (MDC) in Berlin.
“We wanted to disentangle the effect that diseases have on host microbiomes from the effect of medications, particularly in patients taking more than one drug at the same time,” says co-first author Maria Zimmermann-Kogadeeva, group leader and former postdoc at EMBL Heidelberg. “Being part of the MetaCardis consortium enabled us to use multi-omics data from more than 2000 patients with cardiometabolic diseases,” she adds. Moreover, the large sample size enabled the team to demonstrate that the amount of pharmaceuticals provided has a considerable impact on the degree of influence of drugs on the microbiota.
“We know that the microbiome can reflect the status of a patient’s health and provide a range of biomarkers to assess the severity of diseases. What is often overlooked, however, is that the medication used to treat a disease also affects the state of the microbiome,” says Rima Chakaroun, one of the lead authors of the study and a clinician scientist at the University of Leipzig Medical Center. Dr. Chakaroun is currently a postdoctoral fellow at the Wallenberg Laboratory, University of Gothenburg.
A statistical method that accounts for many influencing variables allowed scientists to distinguish the impacts of medications and illness. “We now have a robust methodological framework that makes it possible to get rid of many of the standard errors,” says Professor Bork. “That allowed us to show that medication can mask the signatures of disease and conceal potential biomarkers or therapeutic targets.”
The research draws on the expertise, knowledge, and techniques of professionals from six different nations. “It was very motivating to work with an interdisciplinary team of clinicians, bioinformaticians, and computational systems biologists to advance our understanding of molecular interactions in cardiometabolic disease,” says Dr. Zimmermann-Kogadeeva.
The team anticipates that these findings will aid in medicinal repurposing including the development of personalized treatments and preventative methods.
The results were published in the journal Nature.