Inflammatory bowel disease (IBD) is a painful chronic condition affecting around 3 million Americans. Scientists have yet to find a cure, and current available treatments are either not very effective or can cause harm in ways that makes healthcare professionals concerned for patient wellbeing. A new UT Southwestern study gives hope for improvement in this area, finding that a targetable group of molecules within the gut’s immune cells is responsible for preventing IBD flare-ups.
“We discovered a fundamental mechanism that inhibits inflammation in the gut,” says Venuprasad Poojary, Ph.D., Associate Professor of Internal Medicine and Immunology at UT Southwestern and a member of the Harold C. Simmons Comprehensive Cancer Center. “Understanding these kinds of basic details about the immune system is essential for developing new strategies to treat inflammatory diseases.”
For some time now, researchers have understood that increased levels of IL-7, an immune molecule, is linked to the most severe IBD symptoms. This has prompted drug development targeting the molecule. However, while it has been effective for psoriasis, similar results aren’t seen in IBD patients. Additionally, these drugs may negatively impact immune cells.
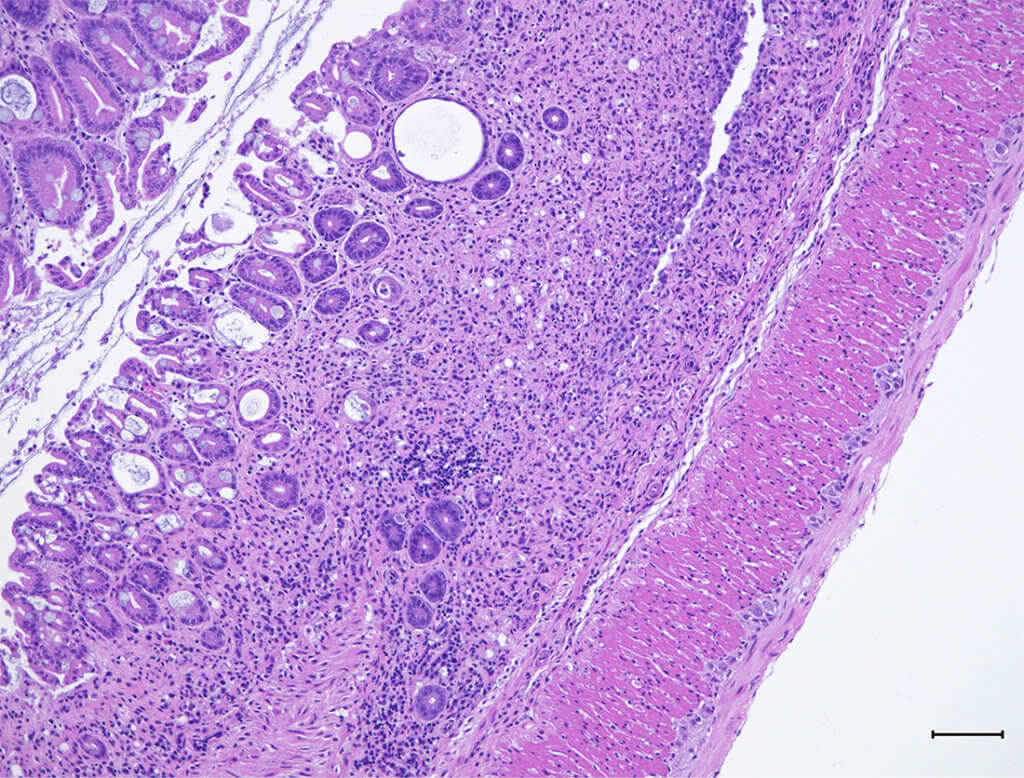
In this research, Dr. Poojary and his team explored other molecular interactions within the inflammatory cells that lead to IL-7 production. They discovered a protein called Pak2 that may be beneficial for this patient population. Upon blocking the protein in mice, the animals experienced weight loss, increased colon inflammation, diarrhea, and bloody stools. All of these lessened when Pak2 was unblocked.
Moreover, extra experiments demonstrated that Pak2 binds to RORgt, which is a protein that activates the IL-17 gene. They found that RORgt can quicken inflammation onset while Pak2 halted it. The team was also able to show that Pak2 can break down RORgt, preventing it from activating IL-17 altogether. “We clearly showed that turning up this pathway can inhibit colon inflammation, and we think this pathway could be targeted to attenuate this inflammation as well,” explains Dr. Poojary.
Future steps involve organizing follow-up studies that can contribute to pharmaceutical advancements that allow Pak2 to shine. Drugs with this target could not only act to relieve patients of pain related to their inflammation, but they could do so without suppressing their immune function and leaving them more susceptible to infection. Their findings could even support clinical care outcomes in other diseases like multiple sclerosis and rheumatoid arthritis, which are two conditions where beneficial treatment remains scarce.
This study is published in the journal Cell Reports.
