Pain-sensing neurons can ward off inflammation and tissue in the gut by regulating the gut microbiome, finds a new mouse study. Researchers at Weill Cornell Medicine observed neurons in the gut releasing a molecule called substance P that prevents further disruption to gut microbes.
People with constant inflammation, such as those with inflammatory bowel disease (IBD) often show low numbers of these pain-sensing nerves.
“These findings reshape our thinking about chronic inflammatory disease, and open up a whole new approach to therapeutic intervention,” said study senior author Dr. David Artis, director of the Jill Roberts Institute for Research in Inflammatory Bowel Disease, director of the Friedman Center for Nutrition and Inflammation and the Michael Kors Professor of Immunology at Weill Cornell Medicine, in a statement.
Defining the relationship between pain-sensing neurons and the gut microbiome can help in understanding the host-microbiota interactions—especially in people with gut-related disorders. IBD, for example, covers both Crohn’s disease and ulcerative colitis. This inflammatory condition afflicts several million people in the United States. Current treatment options target the immune system to dampen the inflammatory response, but more recent research has expanded on the influential role the microbe plays in regulating gut immunity.
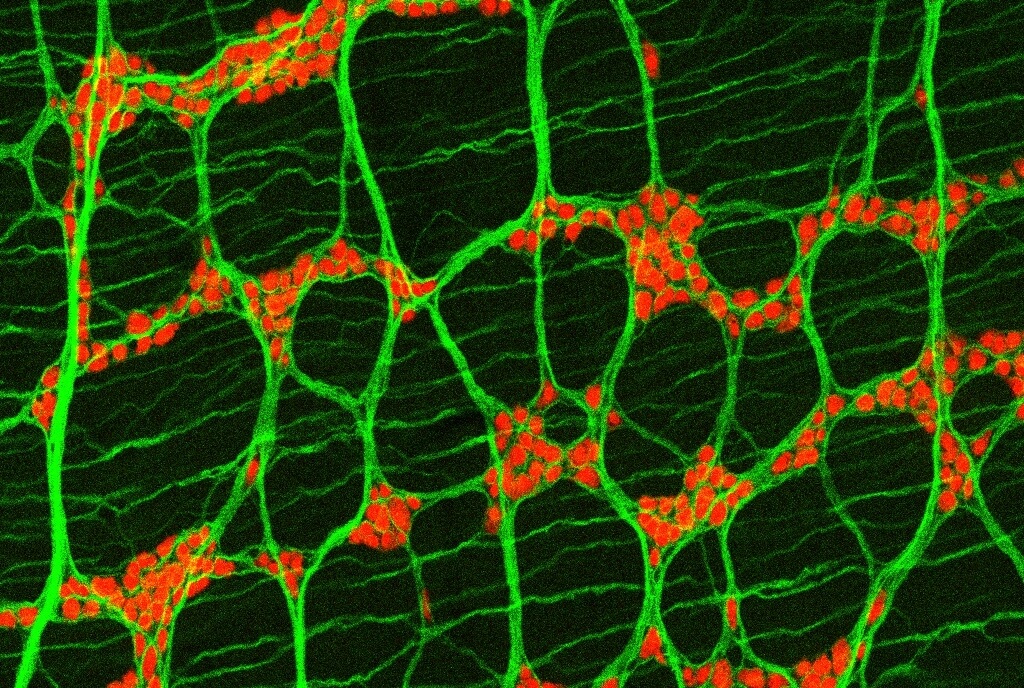
The nervous system is a relatively new addition to the dynamics that go into modulating gut inflammation. In the current study, the researchers inspected pain neurons that extend their nerve endings into the gut.
The pain-sensing neurons connected to the gut are found in the lower spine and express a surface protein known as TRPV1. This acts as a receptor for any pain-related signals in the body. This includes pain from high heat and acidity, which the brain then translates into burning pain. During the study, the researchers found that blocking the TRPV1 receptors in gut nerves caused worse inflammation and tissue damage in IBD mouse models. However, if the receptors were activated, they protected against inflammation.
Mice whose TRPV1 receptors were blocked showed changes in their gut bacteria populations. When this bacterial population was transplanted into normal mice that had their TRPV1 receptors intact, the researchers observed increased susceptibility to inflammation and tissue damage. The antibiotic treatment helped reverse this increased risk of inflammation in both groups of mice, supporting the role of gut bacteria.
One of the reasons why gut bacteria play a large role in regulating inflammation has to do with a molecule nerves secrete called substance P. The team observed substance P helped reverse any harmful effects that were caused by blocking TRPV1. The relationship between neurons and microbes appeared bidirectional. Some bacterial species activated TRPV1-expressing nerves and promoted the release of substance P.
Beyond studying mice, the researchers studied gut tissue collected from people with IBD. They found gut samples had disruptions to TRPV1 and substance P gene activity. In addition, there were fewer signs of TRPV1 nerves present in the gut.
“A lot of current anti-inflammatory drugs work in only some patients, and pharma companies really haven’t known why,” says Dr. Artis. “Maybe it’s because, when it comes to chronic inflammation, we’ve been seeing only some of the picture—and now the rest, including the role of the nervous system, is starting to come into focus.”
The study is published in the journal Cell.