A new Swedish study finds that excluding gluten from the diets of individuals suffering from Irritable Bowel Syndrome (IBS) may not be as important as previously thought. Instead, research is proving another dietary element to be the culprit. Types of carbohydrates known as fodmaps, (Fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) prove to be an aggravation to the gastrointestinal system.
Fodmaps are also commonly found in foods that also contain high levels of gluten, which could be why gluten tends to get the rap for the onset of IBS symptoms. This new study sets out to separate these two parameters and find the side effects of these nutritional elements. Results of studies of this nature show promise in aiding patients with IBS symptoms to differentiate dietary nuances in their daily diets.
Fodmaps versus Gluten Study
Approximately 3 to 5 percent of the global population suffers from IBS in some form. The disorder is complex and has different symptoms such as constipation, diarrhea, or stomach pain and discomfort.
Swedish researchers explore the effects of a gluten-rich study dish and a fodmaps-rich study dish in 110 people diagnosed with IBS over several weeks.
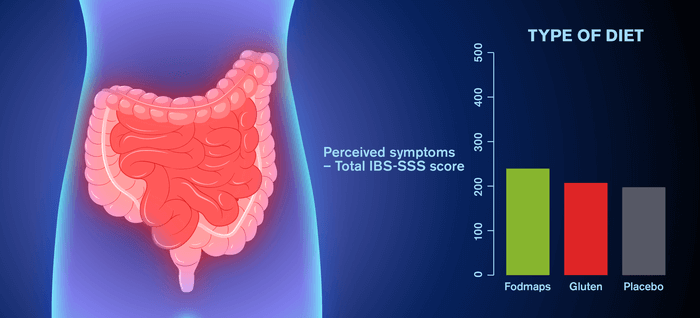
A week at a time, study subjects were fed rice pudding dishes with a high concentration of fodmaps (50g) or rice pudding dishes with a high concentration of gluten (17.3g). The effects of these dishes were compared to a placebo rice pudding dish that contained neither dietary element. The study participants consumed the rice pudding placebo dish and the test dishes in random order. Each subject took a week break between consuming study dish samples. Participants’ average diets consisted of low amounts of gluten and fodmaps throughout the study. After each weekly study session, study subjects provided a blood sample, stool sample, and a symptom questionnaire.
Unique Elements of this Double-Blind Study
Additionally, this study is a double-blind study meaning that neither the research participant nor the study administrator is aware of what participant consumes which dish or at what time.
“Diet studies are difficult to conduct double-blind, as it can often be obvious to the participants what they are eating. This is a big obstacle, as knowledge that something has been added to or removed from the diet can affect the result. The fact that we succeeded in creating diets that were completely blind, together with the large number of participants, makes our study unique,” explains Elise Nordin in a statement. Nordin is the lead author of the study and a Ph.D. student in Food Science at the Chalmers University of Technology.
Dietary Study Results
This study shows gluten to have no unfavorable or measurable impact on the symptoms of the IBS test subjects. The study also finds that fodmaps exacerbate IBS symptoms, however not to the extent that researchers thought.
Researchers find that IBS affects people differently across the board depending upon components of a person’s physiology and mental health. This study is a component within an encompassing study project exploring biomarkers in the gut flora and bloodstream that may predict long-term health outcomes. This broader study gives researchers the ability to categorize individuals into metabotypes, depending upon a person’s metabolism and gut microbiome in reaction to particular diets. Moreover, this research enables experts to determine if these unique groups express different IBS symptoms.
“Finding objective biomarkers that can determine if an individual belongs to a certain metabotype for IBS symptoms could make life easier for many individuals with IBS. There are many indications that it is possible to use objective markers for more individually tailored dietary advice,” explains Professor Rikard Landberg. Professor Landberg leads the Division of Food and Nutrition Science at the Chalmers University of Technology.
Scientists and researchers hope a continuation of these studies will aid individuals with IBS in properly separating dietary components into those that upset the disorder and those with no effect.
This study is published in the American Journal of Clinical Nutrition.

Any relation to dietary Saccharin?
The ‘gluten free’ industry wont like this… / sarc
Oh come on, IBS is from heavy metals, often it’s mercury.
Yes, I agree. Heavy metal gives me gas, too. You should smell my farts when Metallica comes on.
nonsense.
ibs can be affected by those things but its a functional problem. low fodmaps can help. but everyone saying that its caused by something, like heavy metals is wrong. most ibs patients need counseling and stress management strategies, not less mercury.
In the future, victims like you will be sequestered at a camp that plays Donnie and Marie 24/7. Your gas will smell like marshmellows when they are done with you.
jarred funny man
Remember that this is only one study, and many others researcher found different results. There are several aspects of the referenced research that appear suspect, such as claiming only 3 to 5 percent have IBS or similar conditions, no mention of the composition or size of the sample, and the use of rice pudding. Remember that researchers can be bias too. Gluten sensitivity is real, and Celiac disease is real. Millions of people are feeling better and have become healthier because they have eliminated gluten and some other foods from their diet. However, ever person is unique. Genetics make a difference. A person suffering from IBS should following the testing protocol, and try different dietary options to find what is best for them. Also, IBS is a catch-all term that means that the doctors have no idea what is causing the symptoms. Sensitively to fodmaps is nothing new. For some people, eliminating or reducing fodmaps is enough. For others, it is not helpful. The medical community is challenged by so-called IBS and other stomach and bowel problems, because unlike allergic reactions, food sensitives are very difficult to test for.
Thank you, Doug. This is one, very small study that basically proves nothing. The best “research” any of us can do is our own. Pay attention to our bodies and what works and what doesn’t.
I wonder if Valium might help IBS.
That’s not how gluten works. Study is void.
IBS from gluten takes 2 months to recover without a spec of gluten. If you test week by week with random gluten or not, there will be no change. 8 weeks without gluten is needed before reintroduction if you want to see the changes. This study is complete trash. Obviously by an idiot whom knows nothing of gluten, or it’s misleading on purpose.
Feeding both the groups rice pudding may not be the greatest idea as low-carb doctors will tell you that the cause of IBS is processed foods and excess fiber. Humans cannot digest fiber and need to farm out the job to bacteria. Why eat it at all? Dr. Paul Mason shows some interesting studies on IBS on Youtube: the less fiber, the fewer symptoms basically. But of course those studies need to be replicated to see if they hold true.