The cure for diabetes could be sitting in a healthy person’s stool! Researchers found that transplanting microscopic organisms into mice stopped progression of the disease.
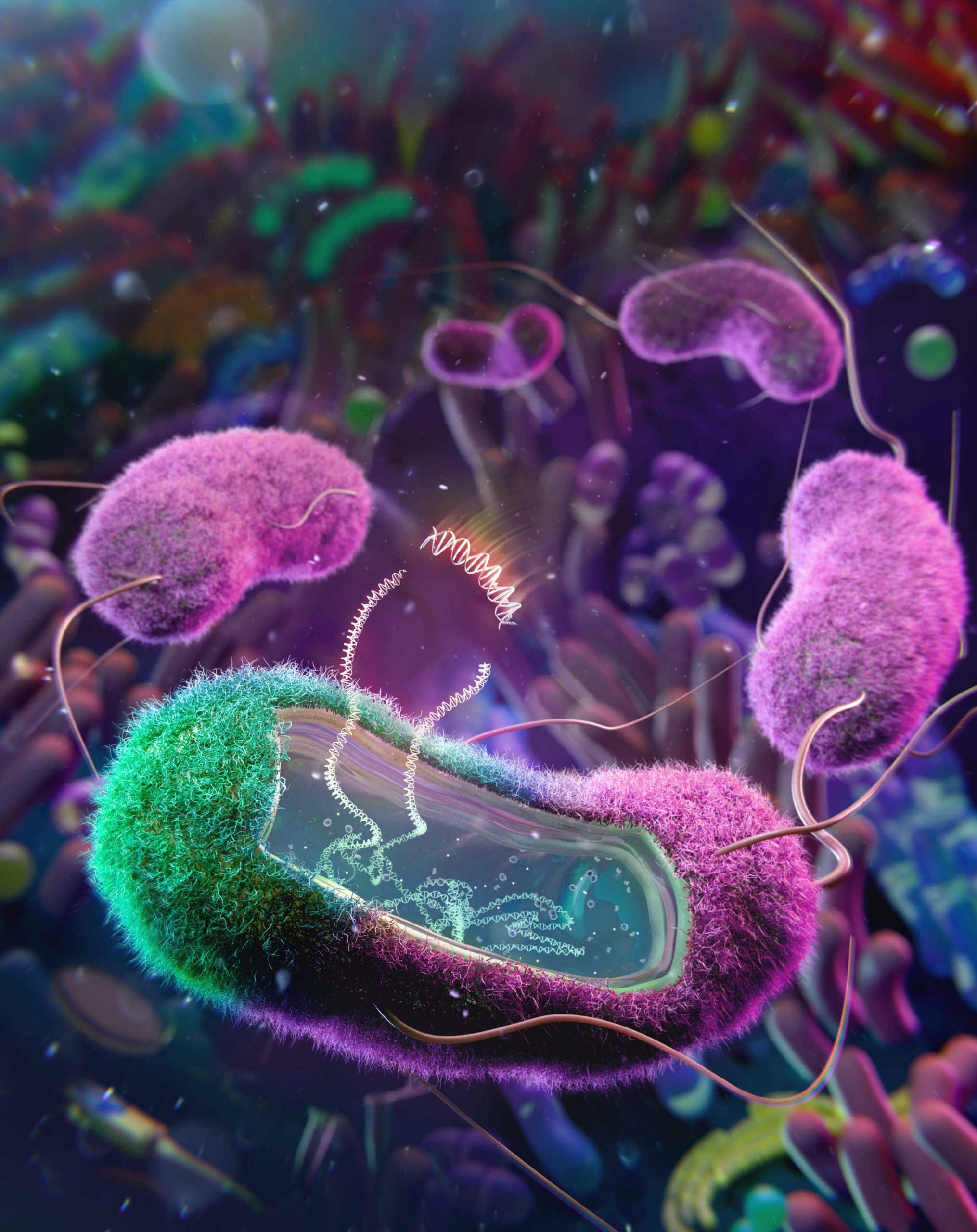
The technique could end the need for painful insulin injections. Specifically, the procedure involves engineering E.coli bacteria from stool samples. They also have the potential to treat a range of gut conditions, ranging from obesity to IBS (irritable bowel syndrome).
“All I can say to the non-native bacteria is good luck. The gut microbiome is very dynamic and is constantly changing, making things even harder for the non-native bacteria,” says senior author Professor Amir Zarrinpar from the University of California-San Diego in a media release.
Scientists have been trying to introduce genetically engineered bacteria into the gut to treat diseases for a long time. In the past, these attempts have focused on engineering common lab strains of E. coli, which cannot compete with the native gut bacteria that are well adapted to their host.
“It is challenging for bacteria that have never lived inside of a mammal before to now go into the gut microbiome jungle with all of these hostile conditions that are geared towards preventing bacterial invaders from taking hold,” adds Zarrinpar, a gastroenterologist at UC San Diego Health.
The UC San Diego team collected E. coli from both human and mice gut microbiomes and added a protein called BSH (bile salt hydrolase). This made the bacteria more robust, extending its survival in the hostile gut environment long enough to treat disease.
“Bacteria in our body are adapted to each one of us specifically: the kind of foods we eat, the common stresses our body experiences or induces, and our genetic background,” Zarrinpar continues. “This constantly fluctuating environment is their normal.”
It is a big advantage for native bacteria and makes them ideal candidates for engineering.
“We have engineered these bacteria to become factories that can live in our microbiome and potentially produce medicines,” the study author explains. “We know that E. coli can pick up pathogenic genes and cause disease, and now we’re just realizing that if we put a beneficial gene in, it can help us to treat chronic diseases, maybe even cure some of them.”
The researchers first collected stool samples from the host and extracted E. coli for further modifications.
“We say to the bacteria: Hey, we will give you a new superpower, which you may not even benefit from, but we will put you right back into the environment that you thrive in.”
Zarrinpar likened BSH to a “superhero.” After a single treatment in mice, the E. coli spread throughout the entire gut, maintaining activity for the entire lifetime of the host.
The study in the journal Cell also showed that the engineered E. coli was able to positively influence diabetes progression in the lab rodents. This is a significant improvement over similar treatments with non-native laboratory strains of engineered bacteria, where patients often require more than one treatment.
Those strains also do not stay in the host’s gut for nearly as long as, or as consistently as, the native E. coli method identified by Prof. Zarrinpar and the team.
In addition to successfully influencing diabetes in mice, the group was also able to make a similar modification to E. coli extracted from the human gut.
Prof. Zarrinpar described the results as “substantial” but there is still more work to do. Engineering native bacteria comes with another set of challenges.
“Native bacteria are very resistant to modifications; it is part of their innate defense mechanism,” the researcher explains.
The data suggests inserting a gene into a native bacterium has a success rate about 100 times lower than doing so with lab strains. However, the researchers are optimizing the process.
“There are many new genetic engineering tools available now that will allow us to engineer these bacteria more effectively,” Zarrinpar says.
The group is planning on using this technology to find ways to treat more diseases.
“We are dreaming big,” Zarrinpar concludes. “This technology is something that can potentially open up the application of the microbiome therapy to influence so many different chronic and genetic diseases.”
Report by Mark Waghorn, South West News Service