Scientists have recently discovered a secret relationship between E. coli bacteria and ileal Crohn’s disease. The findings may provide new areas to target for anti-inflammatory treatment.
Intestinal inflammation caused by Crohn’s disease releases chemicals that benefit the growth and survival of adherent and invasive E.coli (AIEC). AIEC then causes further inflammation to the body.
“This study gives us a whole new patient-based roadmap of things we might want to target to stop Crohn’s-associated E.coli from growing and inciting inflammation,” says senior author Kenneth Simpson, professor in the Department of Clinical Sciences in the College of Veterinary Medicine and at Weill Cornell Medicine in New York City, in a media release.
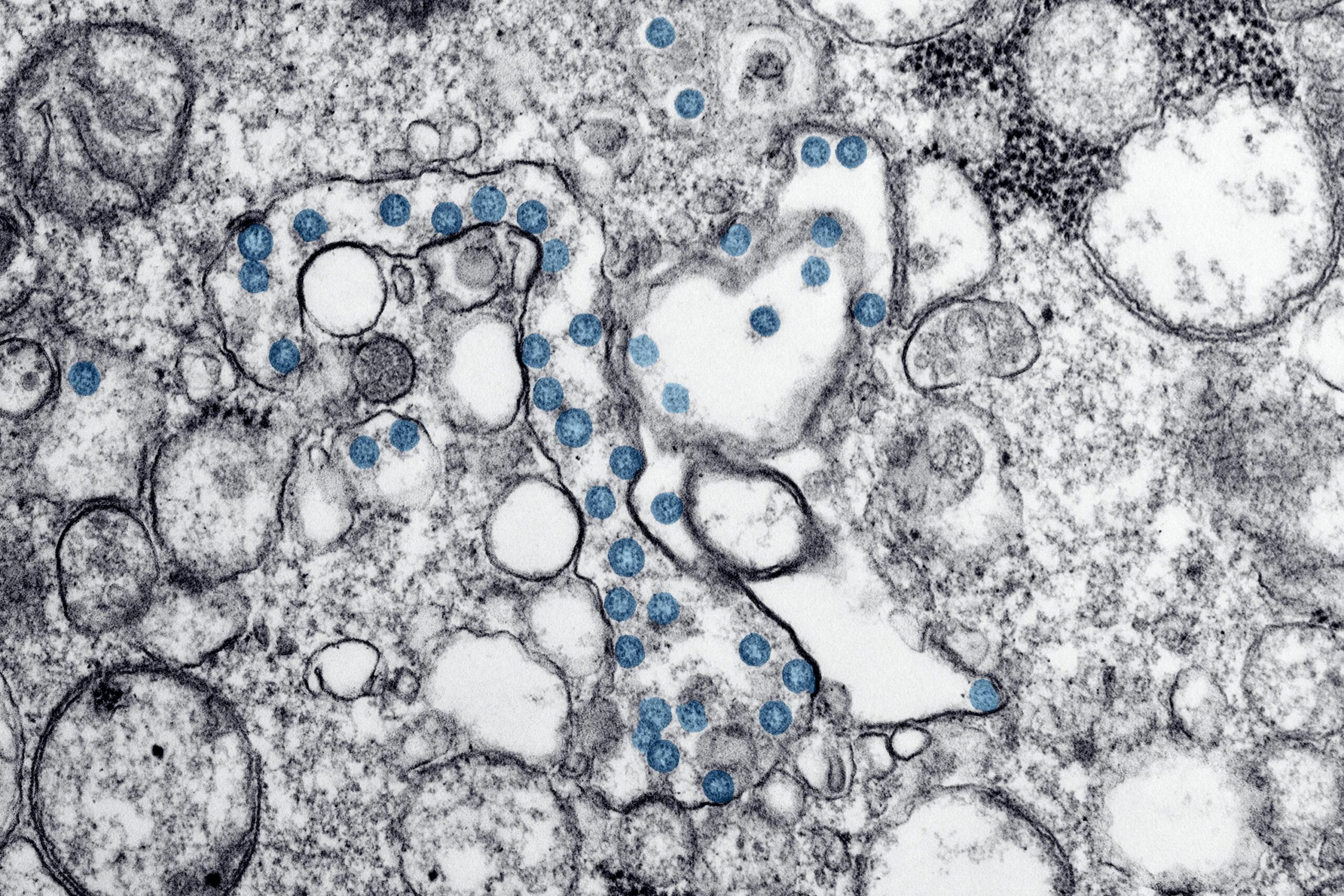
AIEC is a type of E.coli that sticks to and invades epithelial cells from the gut lining. Doing so gives AIEC the ability to replicate in defensive white blood cells. About 21% to 63% of people with ileal Crohn’s disease have shown evidence of AIEC in cultured epithelial cells.
The team profiled the ileal microbiome, chemical environment, bacteria that could be cultivated, and the genetic predisposition of people with and without Crohn’s disease. They wanted to better understand why intestinal inflammation leads to an increase in E.coli.
“Our thought was that this type of E.coli may use substances generated by intestinal inflammation to grow and outcompete other bacteria,” Simpson says. “Essentially we found that the ileal mucosa provides an extensive menu of chemicals that AIEC can mix and match for growth and virulence.”
Results showed that inflammation creates a chemical environment that increases metabolites made up of different phospholipids and amino acids. The uptick in metabolites is used by E.coli as fuel for growth, energy, stress resistance, and movement towards the gut lining. Phospholipids containing ethanolamine and glutamine enhanced AIEC growth in cultured cells.
Previous research has shown that people with ileal Crohn’s disease have genetic mutations that prevent macrophages from eliminating AIEC. The current study adds to the body of literature by linking E.coli growth in the gut to their ability to replicate in macrophages.
“Adherent Invasive E. coli is really hardy and its ability to survive in the inflamed gut, where other bacteria perish, may also enable it to thrive within the macrophages of a Crohn’s susceptible individual, ” says Simpson.
The researchers also found that high levels of E.coli in people with Crohn’s disease makes them more resistant against antibiotics. They suggest indiscriminate antibiotic use could further promote E.coli spreading in the gut, which can then worsen Crohn’s symptoms.
The study is published in the journal JCI Insight.