Deep within the dark, winding corridors of your intestines, a silent, bustling community of trillions of microbes is hard at work. This diverse population, known as the gut microbiota, is more than just a collection of helpful tenants; it’s a vital partner in your health, constantly communicating with your body’s immune system. Now, groundbreaking research is revealing the details of this clandestine conversation, and the findings are nothing short of spectacular. It turns out that a common molecule produced by your gut bacteria is sending a signal to your immune cells, essentially telling them to grow microscopic “tentacles” and reach out to the world beyond your intestinal lining.
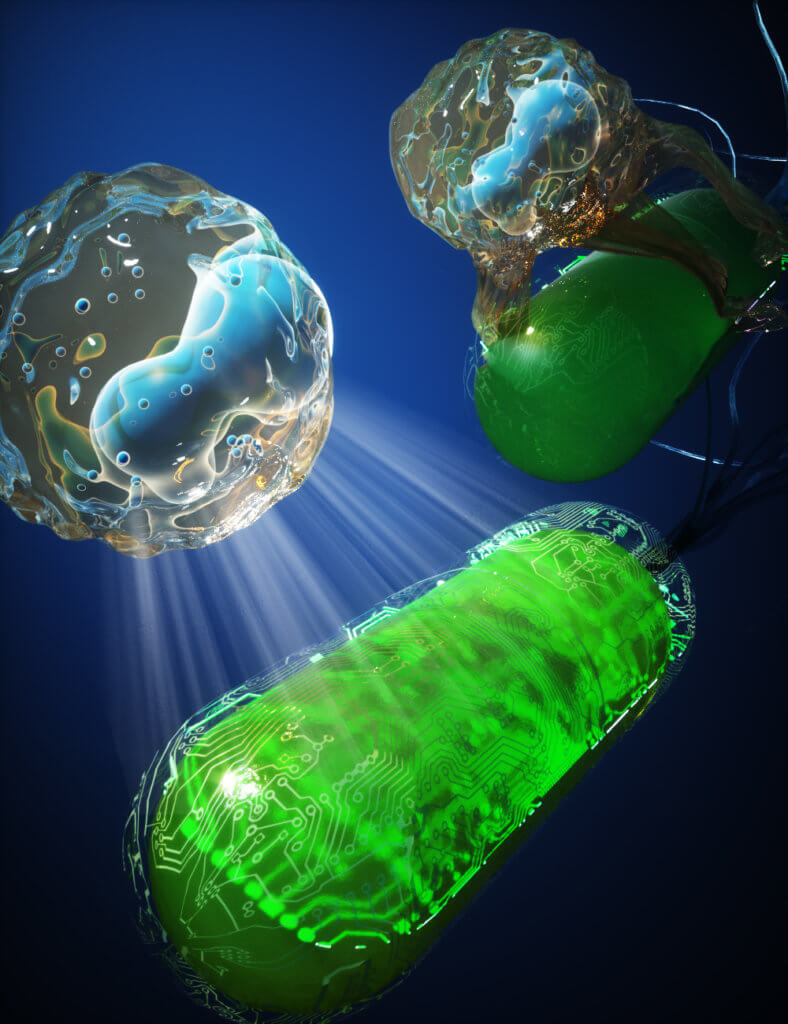
This isn’t a scene from a science fiction movie; it’s the elegant reality of how your body maintains its defenses. A recent paper published in the journal Proceedings of the National Academy of Sciences (PNAS) by a team of researchers from Osaka University has identified a critical pathway in this process. The study shows that a bacterial metabolite, a simple byproduct of digestion called pyruvate, is the key to activating a special receptor on a type of immune cell. This activation causes the cells to dramatically change their shape, extending what the scientists call transepithelial dendrites (TED) through the tiny gaps between the cells that form your gut barrier. These dendrites act like tiny arms, reaching into the intestinal lumen to sample the environment and capture foreign particles, like harmful bacteria or new dietary compounds. By understanding this intricate dance between microbes and our immune cells, scientists are getting closer to developing powerful new therapies, from improving the effectiveness of vaccines to creating new treatments for intestinal infections.
The importance of the gut microbiota in overall health has been a hot topic in medical research for years. We know these microbes affect everything from our metabolism to our mood, and they are especially critical for our immune system. When the delicate balance of the gut is disrupted, it can lead to a host of problems, including inflammatory bowel disease, allergies, and other chronic conditions. A major part of this immune regulation is performed by a family of cells known as dendritic cells (DCs). These cells are like the body’s sentinels; their primary job is to recognize foreign invaders, process them, and present them to other immune cells, like T-cells, to mount a defense. They play a crucial role in distinguishing between a harmless food particle and a dangerous pathogen, a task essential for maintaining what is known as gut homeostasis—a state of healthy balance.
While we’ve known for some time that dendritic cells are active in the gut, the specific environmental cues that influence their behavior in humans have been poorly understood. Previous research in mice had hinted that certain metabolites produced by gut bacteria could promote dendrite formation, but it wasn’t clear if this mechanism was the same in humans. This new research from the Osaka University team, however, provides direct evidence of this phenomenon in human cells, filling a major gap in our knowledge.
To uncover this secret communication network, the research team used a cutting-edge approach that would have been impossible just a few years ago. First, they performed a single-cell analysis on immune cells isolated from the small intestine of four human patients. This technique allowed them to look at the genetic makeup of each individual cell, and they were specifically looking for a family of proteins called G protein-coupled receptors (GPCRs). These receptors are like cellular antennas, specialized to detect specific signaling molecules, including the metabolites produced by gut microbes. The analysis revealed a standout finding: one particular receptor, called GPR31, was highly and specifically expressed on the surface of one type of dendritic cell, known as conventional type 1 dendritic cells (cDC1s). These are the cells that were previously shown to activate a powerful type of immune cell known as CD8+ T cells.
Next, the researchers wanted to see if GPR31 activation was actually responsible for the dendrite formation. To do this, they used a sophisticated coculture system that mimicked the human gut. They grew a monolayer of human intestinal epithelial cells on a membrane, creating a barrier similar to the one in your own body. On the other side of this membrane, they placed the cDC1s. When they added pyruvate, a key metabolite produced by gut bacteria, to the epithelial side, the results were dramatic. The cDC1s began to extend their dendrites, reaching through the membrane to the pyruvate. This dendrite extension was completely dependent on the presence of the GPR31 receptor. To prove this, they also used genetically engineered induced pluripotent stem cells (iPSCs), which are a type of stem cell that can be programmed to become any type of cell in the body. They created cDC1s from these stem cells, with a “switch” that allowed them to turn the GPR31 gene on or off. With the switch on and GPR31 expressed, the cells formed dendrites in response to pyruvate; with the switch off, they did not. This elegant experiment provided a crystal-clear picture of the GPR31 receptor’s crucial role in the process.
The significance of these findings extends far beyond a clever cellular trick. The researchers went on to show that this dendrite-forming behavior directly improves the cells’ ability to fight disease. The cDC1s that extended their dendrites in response to pyruvate were far more efficient at picking up antigens, like a harmless protein called ovalbumin or even killed E. coli bacteria. This improved antigen uptake wasn’t a side effect of general immune activation; in fact, the cells didn’t show signs of being broadly “turned on” by the pyruvate. Instead, the pyruvate-GPR31 signal seems to be a targeted command to change the cell’s physical shape to improve its surveillance capabilities. This mechanism could be a key reason why our immune system is so good at monitoring the gut environment and responding to threats without overreacting and causing inflammation.
This new research reveals a hidden line of communication between our gut microbes and our immune system that we never fully appreciated before. Think of your gut microbes as tiny, helpful scouts, and your immune cells as an army of specialized soldiers. The discovery of the pyruvate-GPR31 axis is like finding the secret radio frequency they use to talk to each other. By better understanding this conversation, we can begin to leverage it for our own benefit. The authors of the study point out that their “results may provide potential targets for clinical applications, such as protection from intestinal infections and improvements in mucosal vaccine efficacy”. In the future, this could mean developing new drugs that target the GPR31 receptor to boost our immune system in the gut, or creating new vaccines that are more effective because they are designed to take advantage of this natural communication pathway. It’s a remarkable step forward in our quest to understand the complex, and often beautiful, biology that makes us who we are.
Paper Summary
Methodology
The research was conducted using human intestinal samples, a 3D culture model, and a human gut organoid coculture system. To identify the relevant receptor, a single-cell RNA sequencing (scRNA-seq) analysis was performed on immune cells from the small intestine of four human patients (n=4). This led to the discovery of the GPR31 receptor on a specific type of immune cell called cDC1s. To study the function of GPR31, the researchers used human induced pluripotent stem cells (iPSCs) to create cDC1s with a “switch” to induce GPR31 expression, allowing them to test the effects of pyruvate in a controlled environment.
Results
The study found that the bacterial metabolite pyruvate specifically activates the GPR31 receptor on cDC1s in the human gut. This activation triggers the cDC1s to extend their dendrites, forming what are known as transepithelial dendrites (TED) that reach across the gut’s epithelial barrier. This process allows the cells to more efficiently capture and uptake antigens, such as dietary compounds and bacterial particles. The research showed that this dendrite formation and antigen uptake was a specific function of the GPR31-pyruvate axis and was not caused by general immune cell activation.
Limitations
The paper notes that studying human cells presents significant challenges. Publicly available single-cell RNA sequencing datasets for human intestinal mononuclear phagocytes (MNPs) are limited. The study’s use of human small intestinal samples was limited to four individuals (n=4).
Funding or Disclosures
The authors of the paper declare that they have “no competing interest”.
Paper Publication Info
The paper is titled “The pyruvate-GPR31 axis promotes transepithelial dendrite formation in human intestinal dendritic cells.” It was published in the journal Proceedings of the National Academy of Sciences (PNAS) on October 21, 2024, and the DOI is https://doi.org/10.1073/pnas.2318767121. The authors are Eri Oguro-Igashira, Mari Murakami, Ryota Mori, and others.