Over the last few years, the importance of intestinal bacteria has been widely discussed. Multiple studies show the symbiotic relationship between the various bacterial species in the gut and certain critical metabolic functions. Bacteria, however, are not the only microbes responsible for the body’s wellbeing. Researchers have found that fungi, another microbe that dwells inside humans, may be just as significant in health and illness as bacteria.
Though bacteria largely overpopulate fungi populations in the gut, fungi can be beneficial to the body. For example, fungi found in the human gut induce certain T helper cells that play a major role in immune functions. However, this inflammatory response can injure the walls of the intestines and cause inflammatory bowel disease (IBD).
In a recent study, Utah University researchers investigated the role of fungi in the gut of mice. Immune cells usually help to maintain a healthy balance in gut microorganisms by keeping fungi from growing out of control. When this balance is disrupted, the immune system is weakened which enables the proliferation of diseases, according to the study.
“Fungi have been wholly understudied in part because they are vastly outnumbered by bacteria,” says June Round, Ph.D., Professor of Pathology at the University of Utah Health and the study’s senior author. “This work adds an important piece to the bigger picture.”
These new findings could lead to new ways to improve gut health with medicines. The research reveals that immunizations may help prevent gastrointestinal illness by boosting the body’s innate immune system to help support a balanced gut microbiome.
A standard diagnostic test for identifying the IBD, Crohn’s disease, detects anti-fungal antibodies, which piqued Round’s curiosity. However, the mechanism through which antibodies alter fungi’s ability to cause illness has not yet been investigated. In an effort to determine the source of the immunological response, the researchers investigated Candida albicans, a type of yeast, and, one of the most prevalent species of fungi in the gut.
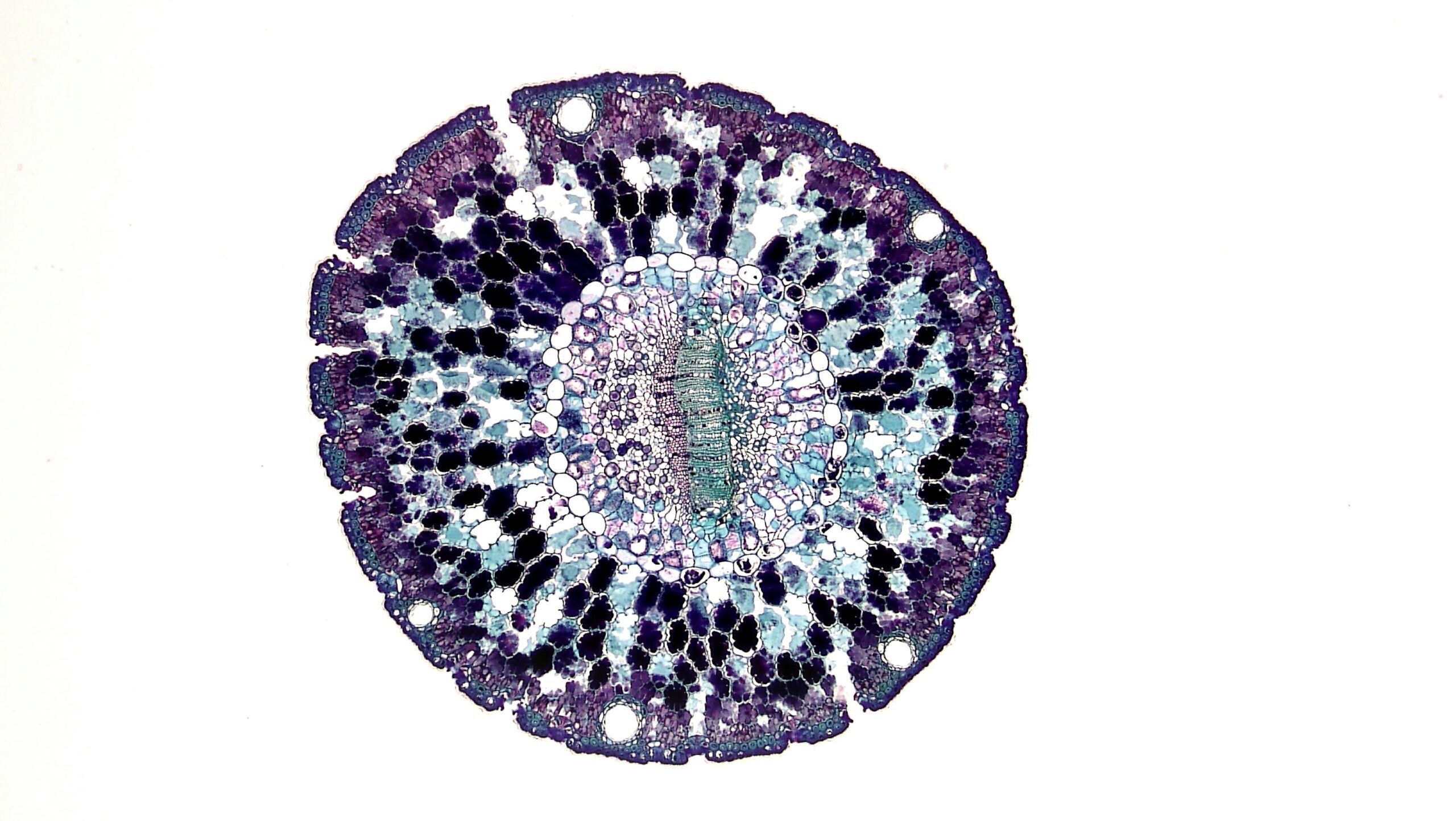
They established via patient samples and mouse experiments that the yeast triggered the highest immune response. Further research revealed that antibodies targeted hyphae, a type of fungal cell with long, branched extensions. Antibodies bind to adhesins, which are proteins that enable microorganisms to attach and enter fungal cells.
Because of this, the team discovered that mice who were colonized with C. albicans in its natural, spherical condition remained healthy. However, mice whose intestines were infected with C. albicans in its aggressive, hyphal form developed symptoms of IBD. This suggests that antibodies in the gut prevent illness by identifying dangerous fungi in their extended form.
In addition to IBD, fungal infections are linked to a wide range of health issues, such as yeast infections in the vagina. In patients with Crohn’s disease, an immune response to adhesin proteins can be generated by an immunization that is now being tested as a treatment for yeast infection. The vaccination reduces the risk of mice developing symptoms of IBD, according to the study.
The team is currently looking into whether vaccinations may be used to aid patients with IBD, as well as if the same strategy could be used to change other microbial populations in the gut. “We aim to exploit interactions with commensal microbes and the host immune system to harness microbial products for therapies,” Round says.
Besides having implications for illness, the results show that fungi may play a role in the maintenance of a healthy gut microbiome. The immune system’s primary function is to prevent illnesses by destroying invading pathogens. When antibodies and fungi connect, it is beneficial for fungi. To better survive in the digestive tract, fungi are prodded out of their obtrusive form and into their spherical, budding form by the immune system.
“The immune system is constraining Candida to its least pathogenic form,” adds Kyla Ost, Ph.D., a postdoctoral researcher in Round’s lab and the study’s lead author. “This is showing us that the communication between host and microbe can be friendly, as opposed to antagonistic, in order to benefit both.”
This study is published in Nature.