Researchers from Children’s Hospital of Philadelphia (CHOP) have made a groundbreaking discovery that could explain why nonsteroidal anti-inflammatory drugs (NSAIDs) can worsen gastrointestinal infections caused by Clostridioides difficile, commonly known as C. diff. This bacterium is the leading cause of antibiotic-associated diarrhea worldwide.
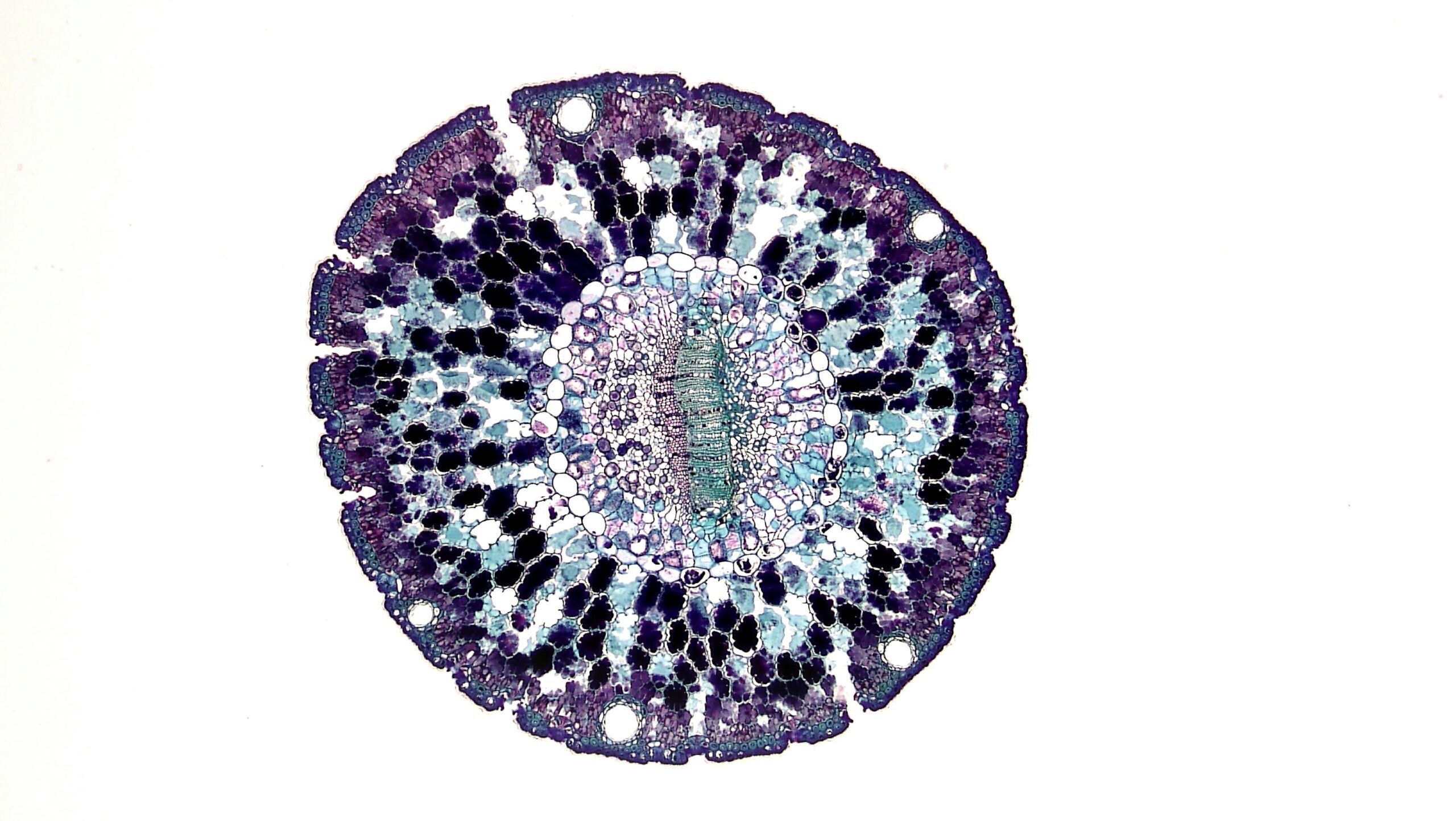
The study highlights how NSAIDs disrupt the mitochondria of cells lining the colon, making them more susceptible to damage from C. diff toxins.
C. difficile infections can range from mild diarrhea to severe and life-threatening conditions, and the factors influencing the varying outcomes have remained largely unclear. However, emerging evidence suggests that diet and pharmaceutical drugs may play a role in both susceptibility to infection and disease progression. The researchers at CHOP sought to understand the impact of NSAIDs on C. diff infection and its potential mechanisms.
Previous studies have shown that NSAIDs, such as aspirin, naproxen, and indomethacin, can negatively affect the gut, causing stomach ulcers and intestinal injuries in conditions like inflammatory bowel disease (IBD). While the effects of NSAIDs on cyclooxygenase (COX) enzymes were known to impair mucosal function in the upper gastrointestinal tract, the researchers explored the off-target effects on cellular mitochondria and how it relates to C. diff infection.
Lead author Joshua Soto Ocaña and his team used in vitro and mouse models to test the permeability of colonic epithelial cells in the presence of the NSAID indomethacin and C. difficile toxins. The results showed that both indomethacin and the toxins increased the permeability of epithelial cells and triggered inflammatory cell death. The combination of the two had an additive effect, suggesting that NSAIDs and C. difficile toxins work together to increase the severity of the infection.
Surprisingly, the researchers found that NSAIDs worsen C. diff infection independently of COX inhibition and instead through off-target effects on mitochondria. When they treated colonic epithelial cells with a molecule similar in structure to indomethacin but without COX inhibitory properties, they still observed cell death. Additionally, adding selective COX inhibitors did not increase cell death, indicating that COX enzyme inhibition is not required for NSAIDs to cause damage during C. diff infection. Instead, the damage occurs through their off-target effects.
Further testing in mice confirmed that both NSAIDs and C. difficile toxins together led to equal enhancement in disease severity and mortality compared to untreated control mice. The researchers also observed similar results when using the NSAID aspirin.
“Our work further demonstrates the clinical importance of NSAIDs in patients with C. difficile infection and sheds light on why the combination of these two may be so detrimental,” says senior author Joseph P. Zackular, PhD, Assistant Professor of Pathology and Laboratory Medicine at CHOP.
These findings provide a crucial insight into the effects of NSAIDs on C. difficile infections, highlighting the potential harm they may cause to patients with these infections. The research also paves the way for further investigation into how NSAID-mediated mitochondrial disruptions could impact other diseases like inflammatory bowel disease and colorectal cancer.
The study is published in the journal Science Advances.