An experimental cancer drug that depletes tumors of their energy supply has the potential to improve the body’s metabolism and control weight gain, among other benefits, according to a recent study. Researchers at Washington University School of Medicine in St. Louis used mice to examine the effects of the investigative cancer treatment that mimics the effects of fasting.
More Than A Cancer Treatment
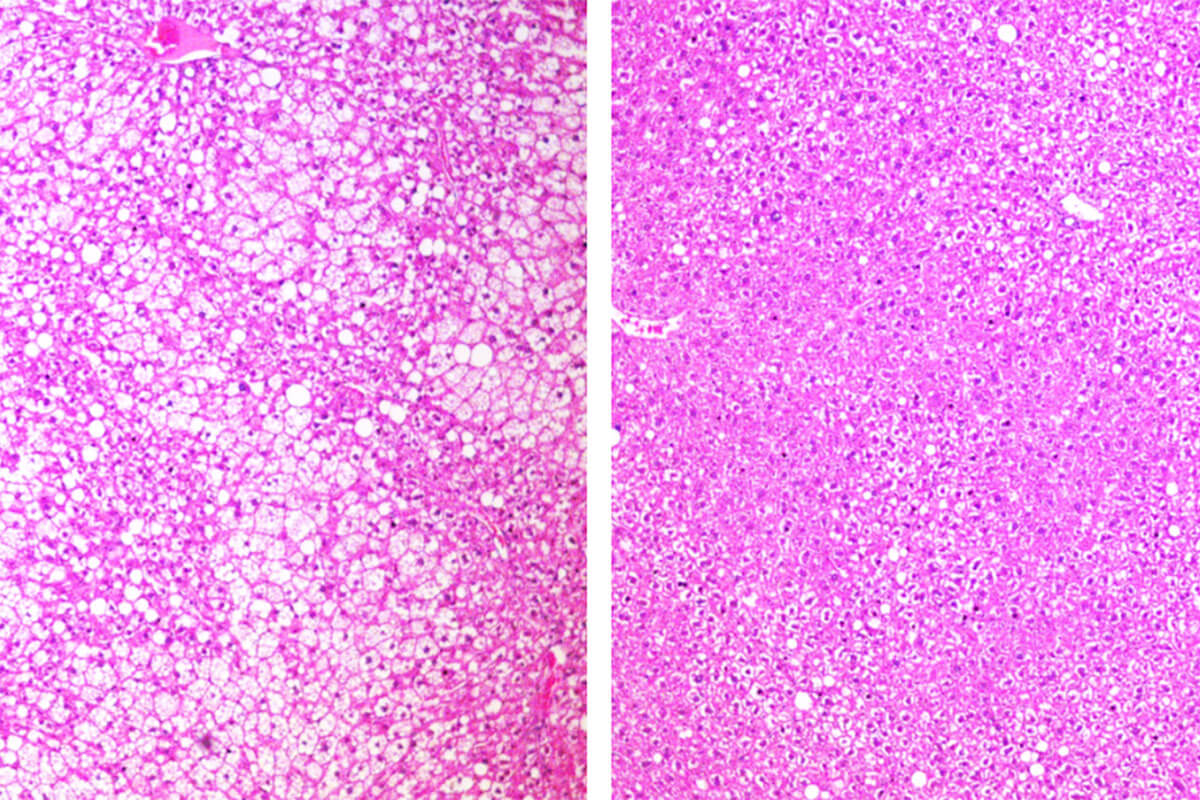
Two different groups of mice were used; one already genetically prone to obesity and another that developed obesity due to a high-fat diet. When treated with the drug ADI-PEG 20, scientists noticed improved cholesterol levels, lower inflammation, and increased insulin sensitivity. The mice predisposed to obesity gained less weight, and the mice fed a high-fat diet were able to lose weight.
Researchers are hopeful that ADI-PEG 20 could potentially be used to treat several different cancers including pancreatic and breast cancers. The drug works by breaking down arginine in the blood, an amino acid that’s an important source of fuel for cancer cells. Interest in the drug was heightened after researchers discovered that the body breaks down arginine much more efficiently when in a fasting state.
Results showed the drug triggers cells to enter a phase known as autophagy. During autophagy, cells burn their own cellular waste for energy since no new energy supply is coming in during fasting. Autophagy is often referred to as “self-eating” because the body is turning inward for fuel sources, rather than digesting outside sources.
“Giving this drug seems to mimic some of the metabolic and therapeutic effects of fasting,” says senior author Brian DeBosch, MD, Ph.D. in a statement. “…We don’t think that the preponderance of the drug’s metabolic benefits are from changes in body weight. In fact, for several outcome measures, the metabolic changes preceded significant changes in weight.”
Long-Term Questions Remain For ADI-PEG 20
Clinical trials have helped scientists analyze the drug’s potential for treating different types of tumors including liver, pancreatic, breast, and prostate cancers. Metabolic therapies, in contrast, tend to have fewer side effects and are much safer than traditional cancer treatments like radiation or chemotherapy. Metabolic therapies are even safer than the newer immunotherapies used to treat cancer.
DeBosch is a pediatric gastroenterologist who hopes to conduct another study to determine whether the drug can increase the metabolism of people who are obese or overweight. But the question of whether the drug is safe to take long term remains to be seen. Because ADI-PEG 20 is a protein, this means patients could develop an immune response, thereby making it ineffective. DeBosch argues there’s a potential role for such treatment during a range of weeks to months.
“Many patients with obesity who are considering bariatric surgery must first lose some weight to make the procedure safer,” says DeBosch. “It can be difficult for such patients to lose up to 10% of their body weight before the surgery. This type of therapy could potentially serve as a bridge to help patients lose weight before bariatric surgery, to reduce the risk of complications during and after the procedure.”
Find this study in the journal Cell Reports Medicine.