In a startling development that could redefine cancer treatment, scientists have successfully engineered a common probiotic yeast to act as a miniature drug delivery system, shrinking hard-to-reach intestinal tumors in mice. This groundbreaking work, out of Washington University School of Medicine in St. Louis, offers a glimmer of hope for a less invasive, oral treatment for challenging gastrointestinal (GI) cancers.
For many, cancer in the digestive system – think stomach, liver, esophageal, pancreatic, or colorectal cancers – presents a daunting battle. These represent more than one-quarter of all cancers, affecting over 5 million people and leading to 3.7 million deaths worldwide each year. Their intricate location often limits the effectiveness of traditional therapies. Even advanced immunotherapies, which aim to rally the body’s own defenses against cancer, struggle to reach these deep-seated tumors when delivered throughout the entire body. But what if the treatment could go directly to the source, bypassing widespread effects? That’s the revolutionary idea behind this new research. Gautam Dantas, PhD, the study’s senior author, explains, “We have engineered a yeast-based probiotic that delivers immunotherapy directly to the tumor site. Our hope is that one day the probiotic could be added to the arsenal of therapies to help shrink tumors in people.”
A Smart Probiotic: The Yeast That Fights Cancer
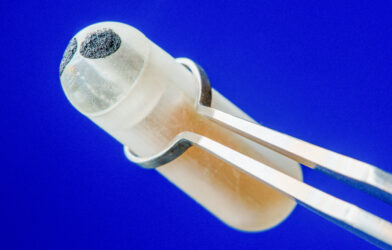
The key player in this medical innovation is Saccharomyces cerevisiae var. boulardii (Sb), a well-known probiotic yeast often found in supplements for gut health. Researchers transformed this beneficial microbe into a tiny factory, equipping it with the genetic instructions to produce and release “miniature” immune checkpoint inhibitors. These special proteins, called haPD-1, are much smaller than traditional immune-boosting drugs.
To understand why “miniature” matters, consider how our immune system normally protects us. It has built-in “brakes” that prevent it from overreacting and attacking healthy cells. Cancer cells often exploit one of these brakes, known as the PD-1/PD-L1 pathway, to evade detection and grow. Immune checkpoint inhibitors work by releasing these brakes, allowing the immune system to recognize and destroy cancer cells. Traditional versions of these drugs are large, making it tough for them to penetrate dense tumors. The smaller, “miniature” versions used here can navigate more effectively into the tumor tissue itself. By having the probiotic yeast create and release these tiny fighters right inside the gut, the researchers aim for a powerful, localized attack.
How the Study Unfolded: Targeting Tumors in Mice
The research team put their engineered yeast, called Sb_haPD-1, to the test in mice that developed colorectal cancer. Notably, these particular tumors were resistant to standard PD-L1 therapy, making the positive outcomes even more significant.
The researchers delivered the Sb_haPD-1 directly to the mice orally. This oral delivery method is a major step forward, as it could eventually replace more invasive treatments. They carefully tracked the yeast’s journey through the mice’s digestive systems, confirming it successfully traveled through the gut, with the highest concentrations observed in the lower part of the small intestine and the colon within one to two hours. Within 12 hours, most of the yeast was no longer detectable, indicating it delivered its therapeutic cargo and then exited the system. This transient presence is a good sign for safety, as it reduces the risk of the yeast staying too long or causing unwanted side effects. The study also verified that a good portion of the yeast survived the harsh environment of the gut, remaining active and able to produce the therapeutic proteins.
Beyond simply reaching the target, the team rigorously checked for any adverse reactions. Mice treated with Sb_haPD-1 showed no notable weight loss, increased mortality, or signs of widespread inflammation. This indicates the treatment was well-tolerated across different mouse models.
Remarkable Results: Tumor Shrinkage and Immune Boost
The most compelling outcome was the direct impact on tumor size. Mice that received the engineered probiotic showed a significant reduction in their intestinal tumors compared to those given traditional immunotherapy delivered throughout their bodies. This finding strongly suggests that getting the immune-boosting treatment directly to the gut tumors can be more effective for these specific cancers.
The treatment also had a noticeable effect on the mice’s immune systems. The scientists observed a decrease in certain immune cells called “tolerogenic T cells” (Tregs) in the lymph nodes near the intestines. Tregs normally put a damper on immune responses, so a reduction in their numbers can free up the immune system to fight cancer more vigorously. There was also a positive trend towards an increase in other beneficial immune cells, called CD4+TNF-α+ T cells, directly within the tumors. These changes in immune cell populations indicate the engineered yeast was successfully fine-tuning the local immune environment to attack the tumors.
Moreover, the study revealed that Sb_haPD-1 treatment significantly altered the balance of bacteria in the mice’s guts, also known as the gut microbiome. While changes to the microbiome can sometimes be a concern, these shifts were not linked to any negative health outcomes for the mice. This opens up new research possibilities into how gut microbes interact with cancer treatments and whether further adjusting them could improve therapy outcomes. The choice to use yeast, rather than bacteria, as the delivery system also offers an advantage by reducing the potential for transferring antibiotic resistance to other gut bacteria.
This research offers powerful evidence for the potential of engineered yeast to change how we approach cancer therapy. It highlights an innovative path toward smart, targeted, and less invasive cancer treatments delivered right where they are needed most. The journey from these promising mouse studies to human clinical trials is a long and complex one, but this study ignites significant hope for a new era in medicine.
Paper Summary
Methodology
Researchers engineered Saccharomyces cerevisiae var. boulardii (Sb), a probiotic yeast, to secrete miniature immune checkpoint inhibitors (haPD-1). This engineered yeast, Sb_haPD-1, was orally administered to colorectal cancer mouse models resistant to standard PD-L1 therapy. The study tracked yeast transit, viability, therapeutic protein secretion, tumor burden reduction, immune cell profile changes, and gut microbiome shifts. Tolerability was also assessed.
Results
Oral Sb_haPD-1 significantly reduced intestinal tumor burden in mice, outperforming systemic immunotherapy. The engineered yeast was viable, stable, and well-tolerated, without causing increased weight loss, mortality, or systemic inflammation. The treatment decreased tolerogenic T cells (Tregs) in mesenteric lymph nodes and showed a trend toward increased anti-tumor T cells in tumors. Additionally, the therapy altered gut microbiome composition without adverse effects.
Limitations
This is a preclinical, proof-of-concept study in mice. Further preclinical testing in diverse mouse models is needed. Observed effects on tumor reduction were statistically significant but modest, suggesting room for future therapeutic improvements. More in-depth mechanistic studies are also required to fully understand immune cell and microbiota modulation. Future advancements could include more precise, targeted drug delivery systems.
Funding and Disclosures
The research received support from various National Institutes of Health (NIH) institutes, including NIAID, NCCIH, NIGMS, NCI, NICHD, and NIDDK, as well as the Radiological Society of North America (RSNA). Several authors hold patent applications related to the yeast-based ICI delivery system.
Publication Information
Rebeck, O.N., Wallace, M.J., Prusa, J., et al. (2025). A yeast-based oral therapeutic delivers immune checkpoint inhibitors to reduce intestinal tumor burden. Cell Chemical Biology, 32, 98-110. Published January 16, 2025. DOI: https://doi.org/10.1016/j.chembiol.2024.10.013.