New research finds that bacteria living in the gut have a way of traveling to the brain and rearranging brain cells involved in anxiety. The mouse study showed gut bacteria caused an increase in anxiety and provide further evidence of the microbiome’s involvement in regulating emotions.
Scientists have known for a while that gut bacteria has a hand in many of the body’s functions, from managing the immune system to helping your metabolism. But in recent years, researchers have dug up evidence of a connection between the microbiome and brain function. This was further highlighted when past studies found people with specific neurological conditions have a different composition for their gut microbiome than healthy people.
“It’s been really difficult to show causation between something that’s happening in the gut and the brain, rather than just associations between the disease states and the presence or absence of certain microbes,” says Brittany Needham, a postdoctoral scholar at California Institute of Technology and first author of the new study in a press release. “We were interested in trying to understand the molecular messages that are going between the gut and the brain, and how these signals may lead to changes in behavior.”
The researchers paid extra attention to a product made from gut bacteria called 4-ethylphenyl sulfate (4EPS). While it’s made in the intestines, evidence shows 4EPS gets absorbed in the blood and travels all over the body of both human and mice. The researchers of this current study previously found high 4EPS levels in mice who had their brains altered to mimic an autistic and schizophrenic brain. A separate analysis in children on the autism spectrum showed that their blood had seven times higher amounts of 4EPS than neurotypical children.
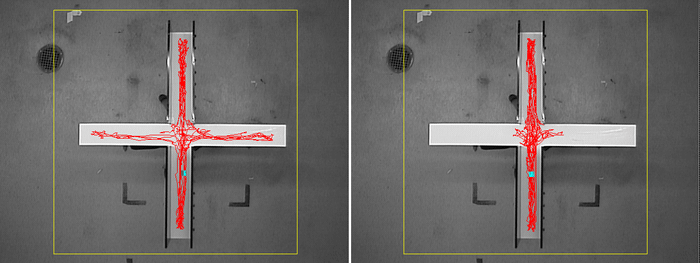
In the current study, the team measured 4EPS levels on a mouse model of anxiety. Two groups of mice had their guts colonized with bacteria, but they genetically engineered one group to not make 4EPS. The mice then underwent anxiety testing. Anxiety in mice is measured through their willingness to explore a new and risky space. Mice that are not anxious will move around and spend their time searching the area, while anxious mice will most likely not move around and linger in the corner.
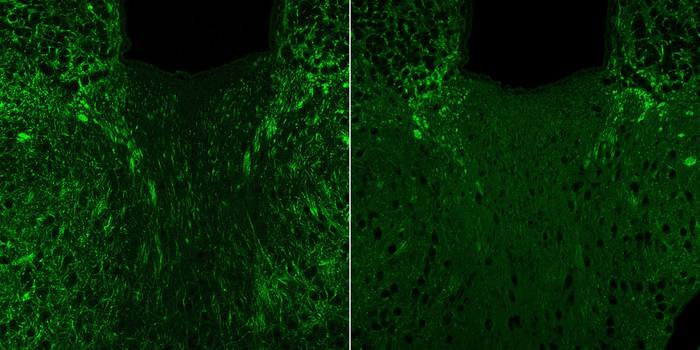
Behavioral tests showed that mice that produced 4EPS had high anxiety, as seen by their reluctance to search a new open space and instead hide. In contrast, mice who were genetically modified to not produce 4EPS were not anxious. Brain imaging confirmed the anxiety behavior, as brain regions associated with fear and anxiety were more activated in mice with 4EPS.
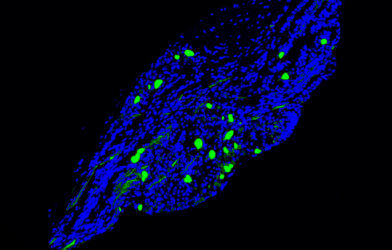
Inspecting the altered brain areas, the researchers found changes in brain cells called oligodendrocytes. These cells have an important role in producing a coating called myelin. Myelin is used to cover and insulate neurons — like the insulating in an electric wire — who are constantly sending electrical messages to other parts of the brain. With higher levels of 4EPS, oligodendrocytes do not grow properly and are unable to make myelin, leaving neurons exposed and vulnerable to damage.
But when mice were given a drug that increases myelin production in oligodendrocytes, the drug helped to override the effects of 4EPS. Drugged mice restored myelin production and anxiety symptoms decreased.
“It’s an exciting proof-of-concept finding that a specific microbial metabolite alters the activity of brain cells and complex behaviors in mice, but how this is happening remains unknown,” says Sarkis Mazmanian, a professor of microbiology and affiliated faculty member with the Tianqiao and Chrissy Chen Institute for Neuroscience at Caltech. “The basic framework for brain function includes integration of sensory and molecular cues from the periphery and even the environment. What we show here is similar in principle but with the discovery that the neuroactive molecule is of microbial origin. I believe this work has implications for human anxiety or other mood conditions.”
The study is published in the journal Nature.