Imagine a tiny, invisible fortress, a slimy shield built by bacteria that makes them practically invincible against our best medicines. This isn’t a scene from a sci-fi movie; it’s the grim reality of “superbugs” like Klebsiella pneumoniae, a pathogen that thrives in hospitals and poses a critical global threat, especially in stubbornly infected wounds. For years, doctors have faced a frustrating battle as these bacteria hide within their protective layers, shrugging off even our most powerful antibiotics.
But what if the key to dismantling these bacterial strongholds wasn’t a complex new drug, but something surprisingly simple, discovered in an unexpected place: the stomach of a cow? Scientists at the Indian Institute of Science (IISc) have just made such a groundbreaking find, unveiling a bovine enzyme that could revolutionize our fight against these formidable infections.
The Superbug Challenge: Unpacking Klebsiella pneumoniae
Klebsiella pneumoniae is an opportunistic bacterium that frequently preys on vulnerable hospital patients, triggering severe conditions like pneumonia and urinary tract infections. It’s particularly notorious for causing chronic, non-healing wounds, especially in individuals with diabetes, sometimes leading to dire outcomes like limb amputation. The World Health Organization has even classified K. pneumoniae as a “critical threat” due to its alarming ability to resist multiple drugs.
This pathogen’s secret to survival lies in its ability to form a “biofilm”—a dense, self-made barrier composed of sugars, fats, proteins, and DNA. This slimy fortress acts as an impenetrable shield, preventing antibiotics and even our body’s immune cells from reaching the bacteria inside. Breaking down this protective layer has been a major hurdle in treating these infections.
A Bovine Breakthrough: Discovering Enzyme GH-B2
The IISc team embarked on a quest for enzymes capable of breaking down complex sugars, known as polysaccharides, which are the primary building blocks of the K. pneumoniae biofilm. They theorized that the bovine rumen—the first stomach of a cow—would be an ideal source. Cows efficiently digest tough plant materials rich in polysaccharides, thanks to a rich community of microbes producing powerful enzymes.
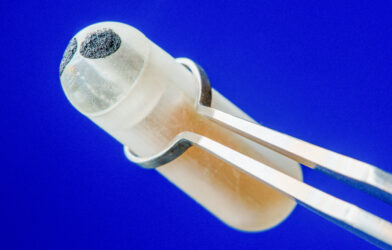
From a pool of 90 enzymes found in the bovine rumen, researchers identified a standout performer: GH-B2. This enzyme, structurally unique with specific “BACON” domains that help it latch onto sugar molecules, proved exceptionally adept at breaking down polysaccharide chains. When produced in the lab, GH-B2 demonstrated remarkable activity and stability, remaining effective across varying pH levels and temperatures—conditions crucial for any potential therapeutic application in the human body.
Dismantling Biofilms and Boosting Antibiotics
GH-B2’s most compelling ability is its power to both prevent new K. pneumoniae biofilms from forming and to dismantle existing ones. The enzyme successfully disrupted established biofilms from various patient-derived K. pneumoniae strains, even at very low concentrations. This action was confirmed by the release of simple sugars, proving GH-B2 was indeed cutting through the biofilm’s polysaccharide matrix. Impressively, it achieved these feats without harming either bacterial or mammalian cells, a critical safety advantage over many current treatments.
The enzyme truly shines when combined with antibiotics. Take meropenem, a common antibiotic often used for serious infections. K. pneumoniae biofilms typically make bacteria highly resistant to meropenem. However, adding GH-B2 dramatically improved meropenem’s effectiveness, reducing the required antibiotic dose to eradicate biofilms by more than tenfold. This shows that by stripping away the biofilm’s protection, GH-B2 exposes the bacteria, making them vulnerable to antibiotics they would otherwise resist.
Real-World Potential: Healing Wounds
To assess GH-B2’s practical application, the scientists conducted studies using a chronic wound infection model in mice. Wounds infected with K. pneumoniae biofilms typically show little improvement with meropenem or GH-B2 alone.
However, when GH-B2 was combined with meropenem, the results were transformative. The combination treatment significantly reduced the biofilm and led to nearly complete clearance of the infection within a week. The treated mice also showed signs of recovery, including weight gain and improved wound healing, evident from the regeneration of healthy skin tissue and new blood vessels. These results underscore GH-B2’s potential to enhance antibiotic treatment in living systems, leading to effective biofilm eradication and promoting healing.
A New Era in Infection Control
The discovery of GH-B2 marks a pivotal moment in the fight against antibiotic-resistant bacteria. By uniquely targeting the biofilm—the very shield that makes these superbugs so formidable—this bovine enzyme offers a biocompatible and innovative strategy to disarm them. Because GH-B2 breaks down the biofilm matrix rather than directly attacking the bacteria, it may be less prone to inducing resistance, a constant concern with traditional antibiotics. This pioneering research, inspired by nature’s own microbial factories, paves the way for exciting new treatments. This enzyme could be a game-changer for severe wound infections, especially in vulnerable individuals, and might even be integrated into medical device coatings to prevent infections from taking hold. The war against superbugs is relentless, but with allies like GH-B2, we now have powerful new tools to win.
Paper Summary
Methodology
This study identified and characterized GH-B2, a bovine rumen microbial enzyme, for its ability to combat Klebsiella pneumoniae biofilms. The enzyme was selected from 90 glycoside hydrolases, expressed in E. coli, and its activity and stability were thoroughly tested. Its ability to inhibit and disrupt biofilms was evaluated against four clinical K. pneumoniae isolates in vitro. The mechanism of biofilm degradation was confirmed via polysaccharide breakdown. Toxicity to mammalian and microbial cells was also assessed. Finally, the enzyme’s synergistic effect with meropenem was examined in vitro and in a mouse wound infection model (5 mice per group), with bacterial load and histopathology assessed over 4 days of treatment.
Results
GH-B2 effectively prevented biofilm formation (IC50 2.50 µM) and degraded pre-formed biofilms (EC50 1.94 µM) by breaking down matrix polysaccharides. It was stable across various conditions and non-toxic. GH-B2 significantly enhanced meropenem’s efficacy, reducing its minimum biofilm eradication concentration by over tenfold. In the mouse wound model, the combination of GH-B2 and meropenem led to near-complete biofilm clearance, reduced bacterial load, and promoted wound healing, confirmed by weight recovery and histopathological improvements. Other enzymes like cellulase showed minimal activity.
Limitations
A limitation of the mouse wound model is the potential for dispersed bacteria to remain localized under the dressing and re-form biofilms, which may explain the lower cell reduction compared to in vitro results. Additionally, the topical application in this model means that complete prevention of biofilm re-establishment isn’t definitively guaranteed, and the enzyme’s contact duration is somewhat unpredictable due to mouse mobility.
Funding and Disclosures
The provided document snippets do not explicitly mention specific funding sources or disclosures for this research paper.
Publication Information
Journal: npj Biofilms and Microbiomes Volume & Issue: (2024) 10:119 Authors: Reshma Ramakrishnan, Abhilash V. Nair, Kirti Parmar, Raju S. Rajmani, Dipshikha Chakravortty & Debasis Das DOI: https://doi.org/10.1038/s41522-024-00593-7 Published in partnership with: Nanyang Technological University Received: 9 April 2024 Accepted: 21 October 2024